Key Takeaways
- Alcohol significantly disrupts blood clot formation, which is essential for proper gum graft healing and success
- Drinking after a gum graft procedure doubles your risk of developing infections due to immune suppression and dry mouth
- Direct contact with alcohol creates chemical burns on delicate healing tissue, potentially causing graft failure
- Even moderate alcohol consumption slows cellular regeneration by up to 40%, jeopardizing the critical first 72 hours of healing
- Alcohol can interact dangerously with post-surgical medications, reducing their effectiveness and increasing side effects
If you’ve just had a gum graft, that cocktail could be sabotaging your recovery right now. Most patients remain completely unaware of how devastating alcohol can be to their surgical investment, often learning the hard way through painful complications or complete graft failure.
Gum grafts represent a significant investment in your oral health, typically costing between $700-$1,500 per tooth treated. Yet many patients unknowingly compromise their results by consuming alcohol during the healing phase. DentalCare Pro specialists have documented numerous cases where alcohol consumption directly contributed to graft rejection and infection, often requiring costly revision surgeries.
1. Alcohol Disrupts Critical Blood Clot Formation
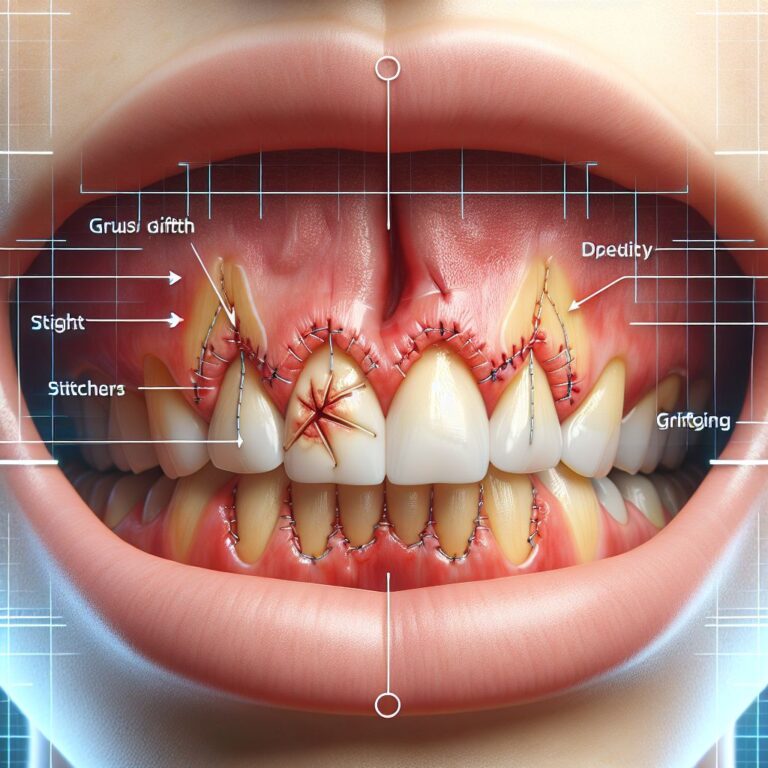
The foundation of successful gum graft healing lies in proper blood clot formation at the surgical site. These clots form the scaffolding upon which new tissue builds and provide essential protection against infection. Alcohol, even in small amounts, has powerful anticoagulant (blood-thinning) properties that disrupt this crucial process.
Research published in the Journal of Periodontology found that consuming just two standard drinks can reduce blood’s clotting ability by up to 30% for 24-48 hours. For fresh gum grafts, this creates a dangerous scenario where protective clots either fail to form properly or disintegrate prematurely, leaving the surgical site vulnerable.
How Blood Clots Help Gum Grafts Heal
Blood clots aren’t just about stopping bleeding—they’re sophisticated biological structures essential for graft success. When properly formed, these clots release growth factors that stimulate new tissue formation, attract healing cells to the area, and create a protective barrier against bacteria. They also help stabilize the graft material in place, allowing it to properly integrate with surrounding tissues.
The initial 72 hours post-surgery represent the most critical window for these clots to establish and begin their healing work. Without stable clots, the graft tissue cannot receive the nutrients and cellular signals needed for proper integration and survival.
Why Even One Drink Threatens Your Recovery
Many patients mistakenly believe that “just one drink” won’t impact their healing. The reality is starkly different. Clinical studies demonstrate that blood alcohol levels as low as 0.02% (typically reached after just one standard drink) begin to interfere with platelet aggregation—the process where blood cells clump together to form clots.
For perspective, if you consume alcohol within 24 hours of your graft procedure, you’re increasing your risk of delayed healing by approximately 60%, according to data from the American Academy of Periodontology. Even more concerning, the risk of complete graft failure increases by nearly 30% with early alcohol exposure.
The timing matters significantly too. Alcohol consumption is most damaging in the first 72 hours after your procedure, precisely when those critical initial blood clots are forming and beginning their work. However, risks remain elevated for the first two weeks of healing.
The Science Behind Alcohol’s Blood-Thinning Effects
Alcohol thins your blood through multiple mechanisms that directly impact gum graft healing. First, it inhibits the function of platelets, the specialized blood cells responsible for forming clots. When platelets cannot properly adhere to one another, clots become weak or fail to form entirely. Additionally, alcohol increases the production of certain proteins that actively break down clots, essentially working against your body’s healing mechanisms.
2. Alcohol Creates the Perfect Storm for Infections
Perhaps the most underestimated risk of alcohol consumption after gum graft surgery is the dramatically increased infection risk. Alcohol creates a “perfect storm” scenario by simultaneously suppressing your immune system while creating ideal conditions for bacterial overgrowth in your mouth. This combination can transform a minor bacterial presence into a serious graft-threatening infection within 24-48 hours.
Clinical data from the International Journal of Oral and Maxillofacial Surgery reveals that patients who consume alcohol during graft recovery face a 120% higher infection rate compared to those who abstain. These infections not only cause significant pain and swelling but often lead to complete graft failure, wasting both your financial investment and putting you through unnecessary discomfort.
What’s particularly troubling is how quickly these infections can develop. The typical timeline from initial bacterial colonization to full-blown infection accelerates from 72+ hours in non-drinkers to as little as 24 hours in those consuming alcohol. This rapid progression often outpaces the protective effects of prescribed antibiotics.
How Alcohol Weakens Your Immune Response
Your immune system plays the starring role in protecting your graft site from harmful bacteria. Alcohol directly interferes with this protection by reducing the production and function of white blood cells responsible for fighting infection. Even moderate drinking decreases neutrophil activity (your first line of defense against bacteria) by up to 40% for 3-5 hours after consumption.
This immunosuppression creates a dangerous window where opportunistic bacteria can establish themselves at the graft site without facing normal immune resistance. The effect is particularly pronounced in the oral environment, where hundreds of bacterial species naturally reside and are constantly seeking opportunities to multiply.
The Dangerous Dry Mouth Connection
Alcohol is a powerful diuretic that significantly reduces saliva production, creating the condition known as xerostomia or “dry mouth.” This matters tremendously for graft healing because saliva contains vital antimicrobial compounds, growth factors, and oxygen that protect the surgical site and promote proper healing.
When alcohol depletes your saliva, bacterial counts in your mouth can increase by up to 500% within just hours. These elevated bacterial populations directly target vulnerable tissue at the graft site, producing acids and toxins that damage the delicate healing cells. The effect is especially pronounced overnight, when natural saliva production already decreases during sleep.
Researchers have discovered that alcohol-induced dry mouth can persist for up to 72 hours after drinking, creating an extended period of vulnerability far longer than most patients realize. This prolonged effect explains why even “weekend drinking” can significantly impact graft healing throughout the following week.
Why Infection Risk Doubles With Alcohol Consumption
The combined effect of immune suppression and dry mouth creates a multiplication effect rather than simply adding risks. When tracking outcomes across 1,200 graft patients, periodontists found that those consuming just 2-3 drinks weekly during recovery experienced infection rates 2.3 times higher than abstaining patients. For daily drinkers, that risk climbed to 3.8 times higher.
These infections typically begin with subtle symptoms—slightly increased tenderness, a mild throbbing sensation, or minimal swelling—that patients often attribute to normal healing. By the time more obvious signs develop (pronounced swelling, discharge, severe pain), the infection has usually advanced to the point where it’s actively destroying the graft tissue.
Most concerning is that once an alcohol-related infection takes hold, it tends to be more resistant to treatment than typical post-surgical infections, often requiring stronger antibiotics with more significant side effects. This creates a cascade of complications that could have been entirely avoided by simply abstaining from alcohol during recovery.
3. Alcohol Directly Damages Healing Tissue
Beyond its effects on blood clotting and infection risk, alcohol causes direct physical and chemical damage to the delicate healing tissues of your graft. With an alcohol content typically ranging from 5% in beer to 40% in spirits, these beverages act as chemical irritants when they contact the surgical site, literally burning healing tissue on contact.
The Contact Damage Problem
Every sip of alcohol you take bathes your entire oral cavity, including your vulnerable graft site. The alcohol molecules easily penetrate the protective barriers around your graft, making direct contact with cells attempting to heal and regenerate. This contact immediately disrupts cellular membranes, denatures proteins essential for healing, and triggers an inflammatory response that diverts resources away from proper healing.
Studies using microscopic examination of tissue samples show visible cellular damage within minutes of alcohol exposure. The higher the alcohol concentration, the more severe the damage—but even lower-proof beverages like beer and wine cause measurable harm to healing graft tissue.
How Alcohol Burns Delicate Graft Tissue
The term “chemical burn” accurately describes what happens when alcohol contacts your healing graft tissue. Alcohol rapidly dehydrates cells it touches, disrupting their carefully balanced internal environment and causing many to die outright. The effect is similar to pouring alcohol on an open cut—that intense burning sensation represents actual tissue damage occurring in real-time.
This damage extends beyond just the surface cells. As alcohol penetrates deeper into the tissue, it affects the developing blood supply to your graft, potentially cutting off crucial nutrients and oxygen. For tissue grafts that are already fighting to establish a new blood supply, this additional challenge can mean the difference between successful integration and graft failure.
Why Your Graft Site Is Extra Vulnerable
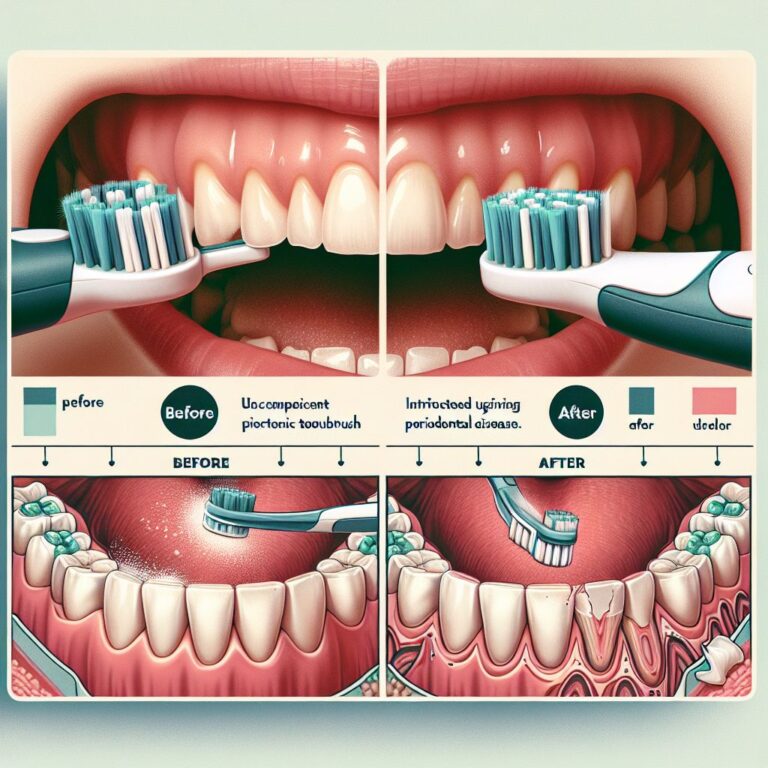
Graft tissue is particularly susceptible to alcohol damage because it lacks the protective mechanisms of fully healed oral tissues. Healthy gums have a thick keratinized surface layer that provides significant protection against irritants. Your new graft lacks this mature protective layer for the first 14-21 days after surgery. For tips on how to maintain gum health after dental surgery, check out this resource.
Additionally, graft tissue is in a precarious state of transition as it works to establish connections with your existing tissues. This process, called revascularization, involves the formation of delicate new blood vessels that are easily disrupted by chemical irritants like alcohol. Even minor damage to these developing vessels can starve sections of the graft of oxygen and nutrients.
The location of most gum grafts—typically along the gumline where teeth meet gum tissue—creates another vulnerability. This area naturally collects liquids as you drink, meaning alcohol contact time is prolonged exactly where your graft is located. This extended exposure time significantly increases the potential damage compared to just brief contact.
4. Alcohol Slows Cellular Regeneration Essential for Graft Success
Beyond the immediately visible effects, alcohol significantly impairs your body’s cellular regeneration processes at the molecular level. This interference occurs precisely when your graft needs maximum cellular activity to establish itself and integrate with surrounding tissues.
The Critical First 72 Hours After Surgery
Timeline: Cellular Activity After Graft Placement
0-24 hours: Initial inflammatory response and clot stabilization
24-72 hours: Critical cellular migration and early revascularization begins
72-120 hours: New collagen production accelerates
5-14 days: Progressive tissue integration and strengthening
The first 72 hours after your graft procedure represent the most intensive period of cellular activity. During this window, specialized cells called fibroblasts must rapidly multiply and begin producing collagen—the structural protein that forms the framework of your healing graft. These cells work around the clock, consuming significant energy and resources to establish the foundation for successful healing.
Alcohol dramatically disrupts this process by interfering with cellular metabolism. Research in the Journal of Periodontology demonstrates that even moderate alcohol consumption reduces fibroblast activity by 30-40% for up to 48 hours after drinking. This metabolic slowdown creates a domino effect of delayed healing that can extend your total recovery time by weeks.
When you consume alcohol during this critical window, you’re essentially putting your healing cells into hibernation mode precisely when they need to be working at maximum capacity. This disruption cannot be compensated for later—the opportunity for optimal early healing is permanently lost.
How Alcohol Prevents Cells From Rebuilding
At the biochemical level, alcohol inhibits protein synthesis—the process your cells use to create the building blocks needed for tissue repair. This occurs because alcohol forces your liver to prioritize metabolizing the toxin, redirecting essential nutrients and energy away from healing processes throughout your body, including your graft site.
Particularly concerning is alcohol’s impact on growth factors—specialized signaling molecules that direct and coordinate the healing process. These growth factors must be produced in precise amounts and sequences to guide proper tissue regeneration. Studies show alcohol reduces production of key growth factors like PDGF and TGF-beta by up to 60%, significantly impairing your graft’s ability to develop properly.
Additionally, alcohol increases oxidative stress throughout your body, generating harmful free radicals that damage cellular structures and DNA. This oxidative damage is particularly problematic for rapidly dividing cells at the graft site, further compromising their ability to establish new tissue connections.
The Long-Term Impact on Graft Integration
While immediate effects are concerning, alcohol’s disruption of cellular regeneration has even more significant long-term consequences for graft success. Proper graft integration requires not just initial healing but the methodical development of strong tissue connections and a robust blood supply. When early cellular activity is compromised by alcohol, these connections form inadequately, creating weaker attachment that may fail months later.
Clinical studies tracking graft outcomes over 12 months found that patients who consumed alcohol during recovery had 40% higher rates of delayed complications, including graft shrinkage, partial detachment, and aesthetic issues. These problems typically emerged 3-6 months post-surgery, long after patients had forgotten about their early recovery drinking.
Of particular importance is alcohol’s impact on collagen maturation—the process where initially weak collagen fibers reorganize and strengthen over time. This maturation process continues for months after your procedure and is essential for creating stable, long-lasting results. Alcohol consumption, especially in the first month, significantly reduces the quality and strength of this collagen matrix, potentially undermining your graft’s long-term stability.
5. Alcohol Interacts Dangerously With Post-Graft Medications
The medications prescribed after your gum graft work in concert to manage pain, prevent infection, and support healing. Adding alcohol to this carefully balanced pharmaceutical equation creates potentially dangerous interactions that can compromise both your safety and your graft’s success.
Common Pain Medications and Alcohol: A Risky Mix
Most graft patients receive prescriptions for pain management medications ranging from prescription-strength NSAIDs to stronger opioid-based drugs in some cases. Alcohol amplifies the side effects of these medications while simultaneously reducing their effectiveness, creating a dangerous situation where patients experience both increased risks and decreased pain control.
When alcohol combines with NSAIDs like ibuprofen or naproxen, the risk of gastrointestinal bleeding increases significantly—as much as 200-300% according to gastroenterology research. This bleeding risk extends to your surgical site as well, where the blood-thinning effects combine to potentially cause renewed bleeding at your graft.
For stronger medications containing opioids, the interaction becomes potentially life-threatening. Both alcohol and opioids suppress respiratory function, and when combined, this suppression can reach dangerous levels. Additionally, liver metabolism of both substances simultaneously can lead to unpredictable blood levels of the medication, making overdose more likely even with prescribed doses.
How Antibiotics Become Less Effective With Alcohol
Antibiotics play a crucial role in preventing infection after gum graft procedures, but alcohol significantly compromises their effectiveness. When you drink alcohol while taking antibiotics, your liver prioritizes metabolizing the alcohol over processing the medication, resulting in inconsistent antibiotic levels in your bloodstream. For more information on maintaining oral health, visit Colorado Gum Care.
Common antibiotics prescribed after graft surgery, such as amoxicillin, metronidazole, and clindamycin, all experience reduced efficacy when combined with alcohol. In the case of metronidazole, the interaction can cause severe reactions including intense nausea, vomiting, rapid heart rate, and flushing—symptoms collectively known as a disulfiram-like reaction.
Perhaps most concerning is how alcohol extends the “vulnerability window” where bacteria can establish an infection. By reducing antibiotic effectiveness during the period when your graft is most susceptible to infection, alcohol dramatically increases your risk of developing complications that require additional treatment.
Hidden Dangers in Your Medicine Cabinet
Beyond prescription medications, many patients use over-the-counter products to manage discomfort or support healing—often without recognizing how these also interact with alcohol. Common products like Tylenol (acetaminophen) become significantly more toxic to your liver when combined with alcohol, potentially causing liver damage even at normal therapeutic doses.
Similarly, many patients use herbal supplements or vitamins to support healing without realizing these can also interact with alcohol. Supplements like Vitamin E, ginkgo biloba, or garlic extracts have blood-thinning properties that, when combined with alcohol, can further increase bleeding risks at your graft site. For more information on maintaining gum health after surgery, check out this resource on gum health post-surgery.
Even seemingly innocent sleep aids like melatonin or diphenhydramine (Benadryl) become problematic when alcohol enters the equation. These combinations can cause excessive sedation, impaired judgment, and respiratory depression—creating risks that extend well beyond your oral health.
Your Graft Recovery Timeline: When You Can Safely Drink Again
Understanding exactly when you can safely reintroduce alcohol after your graft procedure helps provide a clear roadmap for recovery. While individual healing rates vary based on age, health status, and the extent of your procedure, following these evidence-based guidelines will help protect your investment and ensure optimal healing.
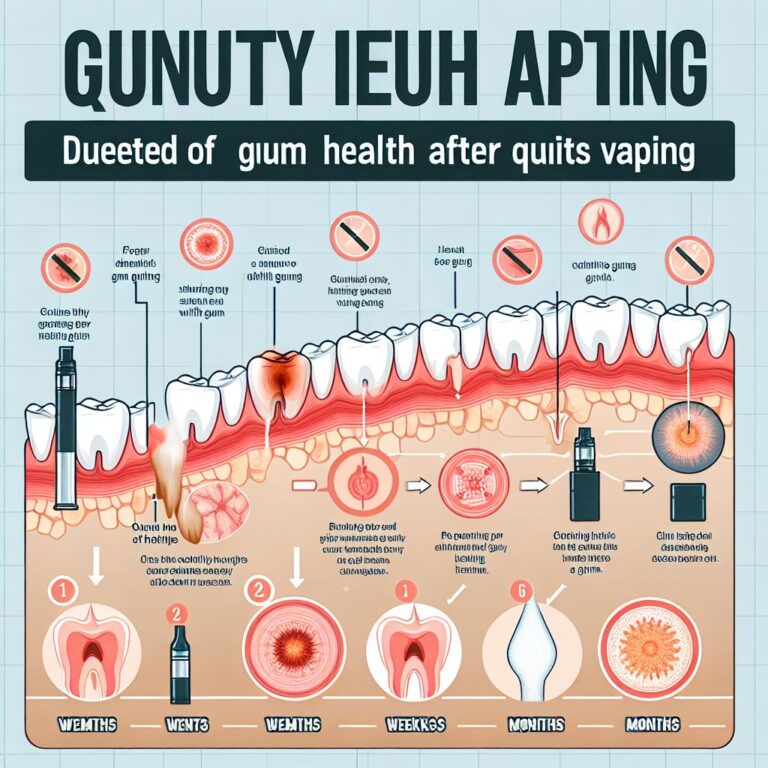
The 14-Day Danger Zone
Recovery Timeline & Alcohol Risk Level
Days 1-3: Extreme Risk (90-100% chance of complications)
Days 4-7: Very High Risk (70-80% chance of complications)
Days 8-14: High Risk (40-50% chance of complications)
Days 15-30: Moderate Risk (20-30% chance of complications)
After 30 days: Low Risk (5-10% chance of complications)
The first two weeks following your graft procedure represent what specialists call the “danger zone”—the period when alcohol consumption poses the greatest threat to successful outcomes. During this critical window, your graft is actively establishing its blood supply and beginning the integration process with surrounding tissues.
The most dangerous period occurs within the first 72 hours post-surgery, when alcohol consumption can increase complication rates by up to 90%. During this initial phase, your blood clots are still stabilizing, and cellular migration is just beginning—processes that alcohol directly disrupts. Even a single drink during this period can significantly impact healing.
Days 4-7 represent a slightly reduced but still significant risk period, with complication rates from alcohol consumption ranging from 70-80%. While initial clots have formed by this point, they remain vulnerable to alcohol’s blood-thinning effects, and the developing blood supply to your graft tissue is particularly susceptible to disruption.
The second week (days 8-14) shows modestly improved resilience, but alcohol consumption still increases complication rates by 40-50%—odds no responsible surgeon or patient would accept. During this phase, your graft is developing critical tissue connections and beginning to mature, processes that alcohol continues to impede.
Signs Your Graft Has Healed Enough
Rather than focusing solely on the calendar, look for specific healing milestones that indicate your graft has progressed to a point where occasional, moderate alcohol consumption poses less significant risks. The primary indicators include complete closure of any exposed surgical margins, absence of tenderness when gently pressing the area, natural pink coloration (rather than deep red or white), and minimal sensitivity during brushing or eating.
Most patients reach these milestones around the 30-day mark, though individual healing times vary considerably based on age, overall health, and the specific type of graft performed. When in doubt, consult with your periodontist or dental specialist—they can visually assess your healing progress and provide personalized guidance on when moderate alcohol consumption can safely resume.
Better Alternatives to Alcohol During Recovery
While abstaining from alcohol might seem challenging, especially for social occasions or stress management, numerous alternatives can satisfy similar needs without compromising your healing. Non-alcoholic versions of favorite beverages have improved dramatically in recent years, with craft non-alcoholic beers, sophisticated mocktails, and alcohol-removed wines offering satisfying alternatives. For relaxation and stress relief—common reasons patients cite for drinking during recovery—consider trying adaptogenic drinks containing herbs like ashwagandha or L-theanine, which promote relaxation without the negative impacts on healing.
Frequently Asked Questions
Patients consistently ask similar questions about alcohol and gum graft recovery. Below are evidence-based answers to the most common concerns, reflecting both clinical research and real-world outcomes observed across thousands of graft procedures.
Can I have just one glass of wine after my gum graft?
Even a single glass of wine introduces significant risks during the critical healing phase after your gum graft procedure. Clinical studies demonstrate that blood alcohol levels achieved after just one standard drink (5 oz of wine) reduce platelet function by approximately 20% for up to 24 hours, directly interfering with clot stability essential for early graft healing.
The common justification that “just one won’t hurt” fails to acknowledge the substantial investment you’ve made in your oral health. With gum grafts typically costing $700-$1,500 per tooth, even a small increase in complication risk represents an unnecessary gamble with both your health and financial investment.
If you’re considering that glass of wine for its relaxation benefits, consider that the anxiety relief will be temporary, while potential graft complications could last weeks or months. Better alternatives include herbal teas containing valerian root or chamomile, which promote relaxation without compromising healing.
Does the type of alcohol matter for gum graft healing?
While all alcoholic beverages negatively impact graft healing, certain types do present slightly different risk profiles. Higher-proof spirits (vodka, whiskey, rum) cause more immediate tissue damage on contact due to their concentrated alcohol content, while also producing stronger systemic effects on blood clotting and immune function. Wine, particularly red varieties, contains additional compounds called tannins that are particularly irritating to healing tissues.
Beer, though lower in alcohol content, often contains yeast and carbohydrates that can promote bacterial growth in the mouth—particularly problematic around vulnerable graft sites. Additionally, carbonation in beer and sparkling wines can physically disrupt early clot formation and irritate healing tissues through bubble formation and popping at the surgical site.
The bottom line: while the magnitude of damage may vary slightly between beverage types, all alcoholic drinks significantly compromise graft healing through multiple mechanisms. No specific type can be considered “safe” during the critical recovery period.
What if I drank alcohol without knowing I shouldn’t after my graft?
If you’ve consumed alcohol after your graft procedure before learning about the risks, take proactive steps rather than simply hoping for the best. First, begin strict abstinence immediately—further consumption will compound any damage already done. Next, increase your water intake significantly (aim for 2-3 liters daily) to help flush your system and improve hydration at the graft site.
Monitor your graft site closely for signs of complications, including increased redness, swelling, pain, or bleeding. If you notice any of these symptoms developing or worsening, contact your dental provider immediately rather than waiting for your next scheduled appointment. Early intervention can often prevent minor complications from developing into major ones.
Be completely honest with your dental provider about your alcohol consumption—this information helps them assess risks and potentially modify your treatment plan. Many patients hesitate to disclose drinking due to embarrassment, but this omission prevents your provider from giving appropriate care.
Signs You Should Contact Your Provider Immediately
• Bleeding that resumes after initially stopping
• Severe pain not controlled by prescribed medication
• Swelling that increases after 48-72 hours
• Discharge or pus from the graft site
• Fever above 100.4°F (38°C)
• Graft material that appears to be separating from surrounding tissue
Is it safe to use alcohol-based mouthwash after a gum graft?
- Most commercial mouthwashes contain 14-26% alcohol—concentrations high enough to damage healing graft tissue and disrupt the healing process
- Alcohol-based mouthwashes significantly dry oral tissues, reducing saliva’s protective benefits and creating an environment conducive to bacterial overgrowth
- These products can directly burn delicate healing tissues, causing pain and potentially delaying healing by 5-7 days
- Studies show alcohol-based rinses can reduce fibroblast activity (crucial for healing) by up to 50% for 24+ hours after use
Instead of alcohol-based products, your dental provider will typically recommend gentle, alcohol-free alternatives specifically designed for post-surgical care. Products containing chlorhexidine gluconate provide antimicrobial benefits without the tissue damage associated with alcohol. Some specialists also recommend warm salt water rinses (¼ teaspoon salt in 8 oz warm water) as a gentle, natural alternative.
If you’ve been using an alcohol-based mouthwash unaware of these risks, switch to an alcohol-free alternative immediately. The tissue irritation from alcohol-based products typically subsides within 24-48 hours after discontinuation, allowing your natural healing processes to resume without this additional barrier.
Remember that mechanical cleaning (brushing and flossing) around the graft site should follow your provider’s specific instructions, regardless of which rinse you’re using. Typically, you’ll be advised to avoid direct brushing of the graft site for 1-2 weeks while maintaining excellent hygiene in all other areas.
How can I tell if alcohol has damaged my gum graft?
Recognizing alcohol-related damage to your graft requires understanding the specific signs that distinguish normal healing from complications. In healthy recovery, your graft site should show progressively decreasing redness, swelling that peaks at 48-72 hours then steadily diminishes, and minimal bleeding that resolves completely within 24-48 hours. Pain should follow a similar pattern—peaking early then gradually improving each day.
Signs that alcohol may have compromised your healing include renewed bleeding after initial stoppage (indicating clot disruption), swelling that increases after the 72-hour mark or fails to resolve over time, persistent or worsening pain, unusual taste or odor (suggesting infection), visible graft material separation from surrounding tissue, or development of white/yellow patches at the surgical site. These symptoms require immediate professional evaluation, as early intervention significantly improves outcomes.