Key Takeaways: Protecting Your Gum Graft
- Gum graft failure occurs in only 5-10% of cases when proper protocols are followed, making it a highly successful procedure overall.
- The first 72 hours post-surgery represent the most critical period for graft survival, requiring strict adherence to aftercare instructions.
- Smoking, diabetes, certain medications, and mechanical trauma are leading causes of graft failure that can be mitigated with proper planning.
- Warning signs of a failing graft include excessive bleeding, severe pain after 3 days, graft tissue turning white or black, and fever.
- Specialized periodontal practices like Coast Periodontics & Dental Implants implement comprehensive prevention protocols that significantly reduce failure rates.
When it comes to repairing receding gums, few procedures are as effective as gum grafting. But the thought of your graft failing can cause serious anxiety. The good news? With proper care and technique, gum graft failure is actually quite rare. At Coast Periodontics & Dental Implants, we’ve developed specific protocols to ensure optimal results, having performed thousands of successful grafts with minimal complications. Understanding what can go wrong is your first step in preventing problems.
Gum grafting offers a proven solution for receding gums, protecting vulnerable tooth roots and restoring your smile’s appearance. The procedure involves transferring healthy tissue to areas where gums have receded, creating a natural-looking barrier that shields sensitive tooth roots from bacterial invasion and further recession.
What Actually Constitutes a Failed Gum Graft
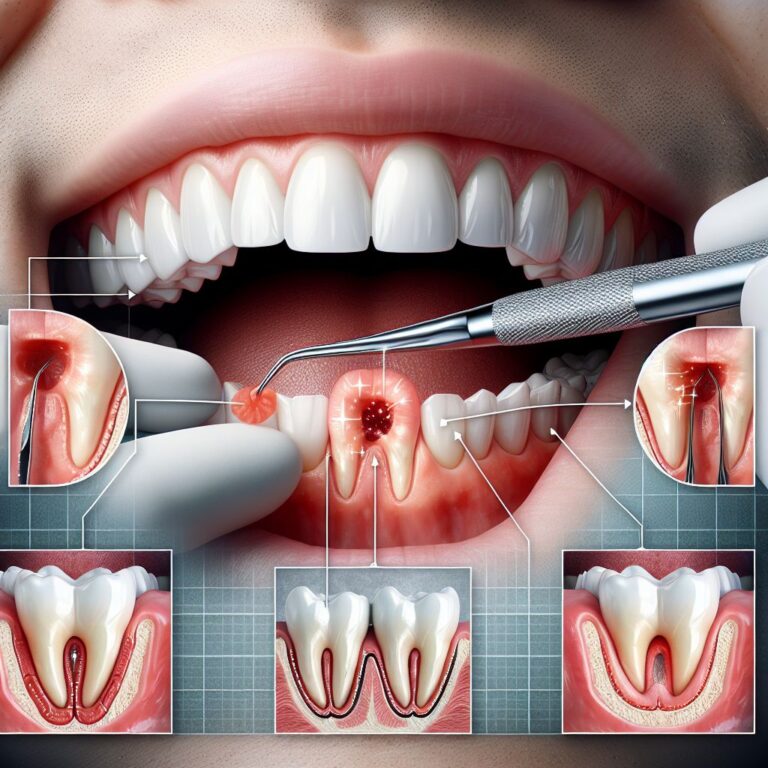
A gum graft failure occurs when the transplanted tissue doesn’t properly integrate with the recipient site. This typically manifests as tissue necrosis (death), significant shrinkage, or complete detachment from the recipient site. Partial integration, where some of the graft takes but doesn’t achieve complete coverage, is generally considered a partial success rather than a complete failure.
In clinical terms, failure means the graft doesn’t achieve its intended purpose – whether that’s covering exposed tooth roots, adding tissue thickness, or halting progressive recession. The tissue may appear discolored (white, gray, or black), feel mobile when gently touched, or develop an infection at the surgical site.
Key Statistics on Success vs. Failure Rates
Research consistently shows that gum grafting enjoys high success rates in the hands of experienced periodontists. According to peer-reviewed studies, the overall success rate for connective tissue grafts – the most common type – ranges between 90-95% when performed by specialists. Free gingival grafts show similarly impressive outcomes with success rates of 85-90%, while pedicle grafts top the list at 95-98% success when proper case selection is applied.
These statistics highlight an important reality: gum graft failure is the exception, not the rule. When failures do occur, they’re often linked to preventable factors rather than inherent problems with the procedure itself. The highest success rates are seen in non-smokers with good overall health who carefully follow post-operative instructions.
Normal Healing vs. Warning Signs of Trouble
Understanding the difference between normal healing and warning signs is crucial for early intervention. Normal healing typically involves mild discomfort that gradually improves, minimal bleeding that stops within 24 hours, and tissue that appears slightly red but progressively becomes pinker over the first week.
Warning signs that differentiate from normal healing include persistent bleeding beyond 24 hours, severe pain that worsens rather than improves after 72 hours, tissue that appears white or black (indicating poor blood supply), significant swelling that increases after the third day, and any signs of infection like fever or pus formation. If you notice these warning signs, contacting your periodontist immediately can mean the difference between saving and losing your graft.
5 Main Reasons Why Gum Grafts Fail
While gum graft failures are uncommon, understanding the primary causes helps patients and practitioners work together to minimize risks. Most failures stem from one of five key factors, often interacting with each other. By addressing these risk factors proactively, we can significantly reduce the already low chance of complications.
- Poor blood supply to the grafted tissue
- Infection at the surgical site
- Patient-related factors (smoking, diabetes, medications)
- Mechanical trauma during healing
- Surgeon experience and technique issues
1. Poor Blood Supply to the Grafted Tissue
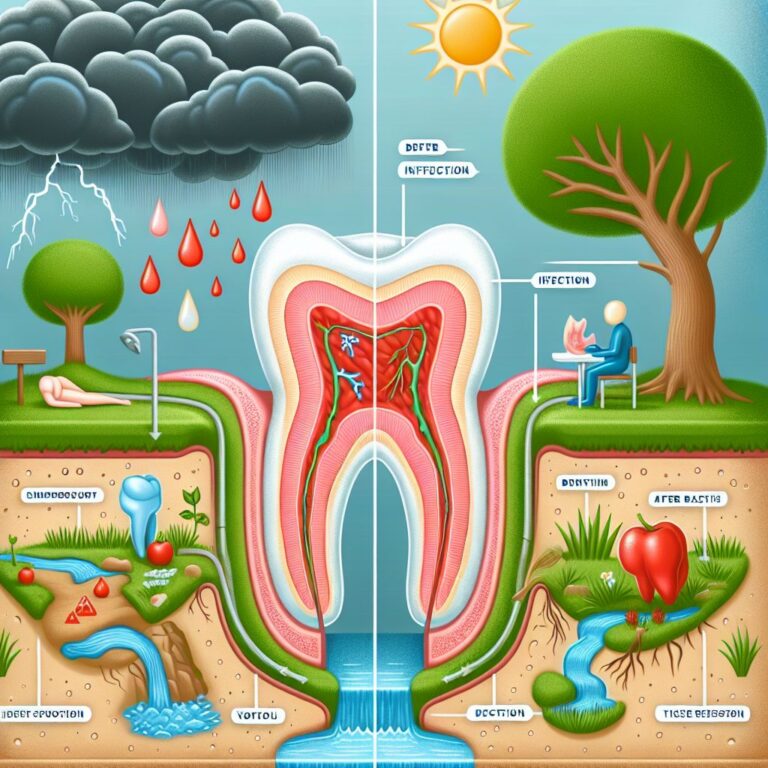
Adequate blood supply is the lifeblood of graft success – quite literally. Without proper vascularization, the transplanted tissue cannot receive the oxygen and nutrients needed for survival. Thin gum tissue at the recipient site, excessive tension on the graft, or improper surgical technique can all compromise blood flow to the new tissue.
To optimize blood supply, experienced periodontists carefully evaluate tissue thickness before surgery, create proper recipient bed preparation with adequate bleeding points, and ensure tension-free suturing. In some cases, a two-stage approach may be recommended for severely thin tissues, first building up the tissue bed before attempting root coverage.
2. Infection at the Surgical Site
Bacterial contamination represents one of the most significant threats to graft success. The oral environment naturally contains billions of bacteria, and when these microorganisms infiltrate the surgical site, they can trigger inflammation and tissue breakdown. The risk increases in patients with existing periodontal disease, poor oral hygiene, or compromised immune systems.
Prevention starts before surgery with thorough cleaning and disinfection protocols. Many periodontists prescribe antimicrobial rinses like chlorhexidine before and after surgery, along with prophylactic antibiotics in high-risk cases. Post-surgical infection control includes careful oral hygiene instructions that balance keeping the area clean without disrupting the healing tissue.
3. Patient Factors (Smoking, Diabetes, Medications)
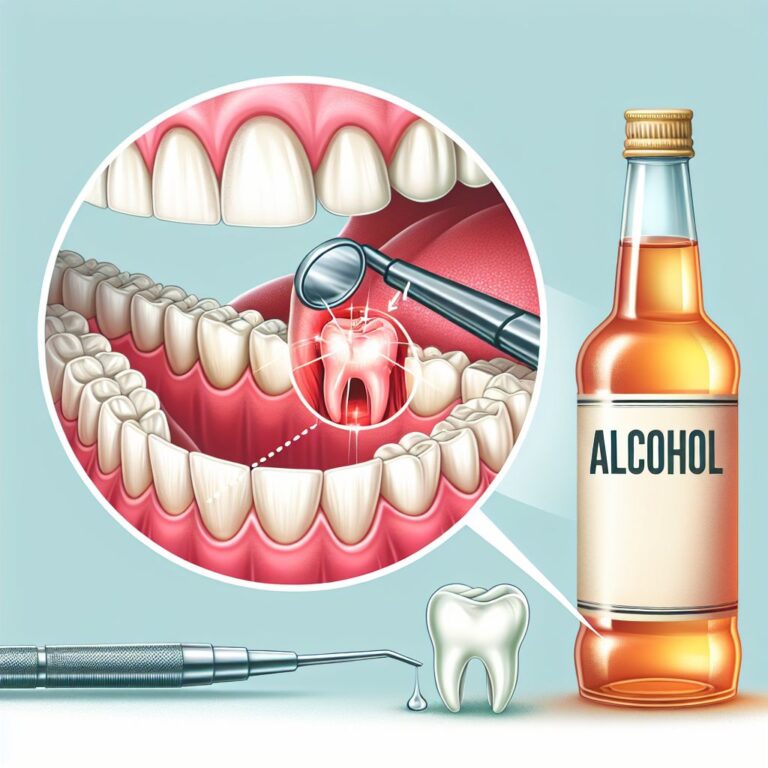
Certain patient-specific factors significantly impact graft healing. Smoking tops the list as the most detrimental habit, reducing success rates by up to 50% through vasoconstriction, reduced oxygen levels, and impaired immune response. In fact, many periodontists refuse to perform grafting procedures on patients who won’t commit to quitting smoking at least two weeks before and after surgery.
Uncontrolled diabetes similarly compromises healing by impairing blood vessel formation and increasing susceptibility to infection. Certain medications like blood thinners increase bleeding risk, while immunosuppressants and some bisphosphonates can interfere with tissue regeneration. A comprehensive medical history review helps identify and address these risk factors before proceeding with surgery.
4. Mechanical Trauma During Healing
The delicate graft tissue is particularly vulnerable to mechanical disruption during the early healing phase. Actions as seemingly minor as aggressive tooth brushing, flossing near the surgical site, or even excessive talking or smiling can dislodge the graft before it fully integrates. Dietary choices matter too – hard, crunchy, or sticky foods can directly damage the graft or create pressure that compromises blood supply.
Successful patients follow strict activity modifications during the critical first two weeks. This typically includes avoiding brushing the surgical area (using prescribed rinses instead), consuming only soft foods, limiting physical exertion, and sometimes wearing a surgical stent or protective appliance over the palate donor site if applicable.
5. Surgeon Experience and Technique Issues
The skill and experience of your periodontist directly impacts graft outcomes. Technical aspects like graft thickness, tissue handling, suturing technique, and proper case selection all influence success rates. An experienced surgeon knows which graft type works best for different clinical scenarios – whether that’s a connective tissue graft for root coverage, a free gingival graft for tissue augmentation, or a pedicle graft when local tissue availability permits.
When selecting a provider, look for board-certified periodontists who perform grafting procedures routinely, not occasionally. Ask about their specific experience with your type of case and their typical success rates. The investment in specialized care often translates to significantly better outcomes and reduced risk of failure.
Red Flags: How to Spot a Failing Graft Immediately
Early identification of a failing graft can mean the difference between salvaging the procedure and needing to start over. Being vigilant during the post-operative period allows for prompt intervention when problems arise. Most complications occur within the first 14 days, with the first 72 hours being especially critical. For more detailed information on gum grafting, you can visit Colorado Gum Care.
The Critical First 72 Hours After Surgery
The first three days post-surgery represent the window when the graft is most vulnerable. During this period, the tissue relies on plasma circulation (fluid absorption) rather than blood vessel formation for survival. Excessive bleeding, significant swelling, or severe pain during this timeframe warrants immediate attention from your periodontist. Following post-operative instructions meticulously during this phase is non-negotiable for graft success.
Patients should monitor for excessive bleeding that doesn’t respond to gentle pressure with a gauze pad, unusual swelling that continues to increase rather than stabilize, severe throbbing pain unrelieved by prescribed medications, or any signs of allergic reaction to medications. These symptoms should trigger an immediate call to your surgeon rather than waiting for your scheduled follow-up appointment.
Visual Changes That Signal Trouble
Warning Signs of a Failing Graft
Color changes: Tissue turning dark blue, black, or bright white
Position changes: Graft shifting position or appearing loose
Texture changes: Tissue appearing slimy, overly wet, or excessively dry
Size changes: Significant shrinkage within the first week
Drainage: Presence of pus or foul-smelling discharge
Visual inspection provides crucial clues about graft health. A healthy graft typically appears slightly red initially, gradually transitioning to pink as healing progresses. In contrast, a failing graft may display concerning color changes – turning very white (indicating poor blood supply), dark blue/purple (suggesting blood pooling beneath the tissue), or black (signaling tissue death).
Another visual warning sign is graft mobility or displacement. The graft should appear stable and well-adhered to the recipient site. If you notice the graft shifting position, lifting at the edges, or seeming detached, contact your periodontist immediately as repositioning may still be possible if caught early enough.
Tissue texture changes also provide important diagnostic information. A healthy graft should maintain a relatively consistent appearance, while failing grafts often develop an abnormal texture – appearing excessively dry and crusty or unusually wet and slimy. These changes frequently indicate infection or tissue breakdown requiring prompt intervention.
Pain Patterns That Aren’t Normal
Pain following gum graft surgery typically follows a predictable pattern – most intense during the first 48 hours, then gradually diminishing over the next several days. Pain that increases after day three, becomes sharply more intense, or develops a throbbing quality often indicates complications such as infection or pressure beneath the graft.
The character of pain matters as much as intensity. Normal post-surgical discomfort tends to be dull and responsive to prescribed pain medications. In contrast, sharp, shooting, or radiating pain that emerges days after surgery suggests nerve involvement or infection. Similarly, pain that suddenly returns after initially improving warrants immediate professional attention.
Our 3-Phase Approach to Preventing Gum Graft Failures
Successful gum grafting requires a comprehensive approach that extends far beyond the surgical procedure itself. Our prevention strategy encompasses three distinct phases, each addressing critical aspects of treatment success. This systematic method has allowed us to achieve success rates well above national averages, even in complex cases with multiple risk factors.
Phase 1: Pre-Surgical Planning and Patient Selection
Prevention begins weeks before the actual procedure with thorough assessment and preparation. We perform comprehensive periodontal examinations to evaluate tissue quality, recession patterns, and underlying causes of recession. For patients with active gum disease, we complete preliminary periodontal therapy to establish a healthier baseline before attempting grafting.
Patients with significant risk factors like smoking, uncontrolled diabetes, or certain medications require special consideration. We may recommend smoking cessation support, glucose control optimization, or medication adjustments in consultation with your physician. In some cases, we suggest delaying the procedure until modifiable risk factors can be addressed, significantly improving the probability of success.
Thorough pre-surgical planning includes detailed measurements of recession depth and width, assessment of available donor tissue, and selection of the most appropriate grafting technique for your specific situation. This preparation phase typically includes custom surgical guide fabrication for complex cases, ensuring precise execution during the procedure.
Phase 2: Advanced Surgical Techniques We Use
Our surgical approach employs evidence-based techniques shown to maximize graft success. For connective tissue grafts, we utilize tunnel techniques that minimize flap reflection and preserve blood supply to the recipient site. This approach reduces trauma and accelerates healing compared to traditional methods. When appropriate, we incorporate platelet-rich fibrin (PRF) – a concentration of your own growth factors – to enhance revascularization and tissue integration.
Technical refinements like microsurgical instrumentation allow for more precise tissue handling, while magnification enables meticulous suturing with minimal tissue trauma. We carefully match graft thickness to recipient site requirements, avoiding overly thick grafts that may struggle to receive adequate blood supply or excessively thin grafts that provide insufficient coverage.
For complex cases, we sometimes employ a staged approach rather than attempting complete correction in a single procedure. This allows initial revascularization and tissue maturation before additional grafting, significantly improving outcomes in challenging scenarios with minimal existing tissue. For more information on these procedures, you can explore our services.
Phase 3: Our Structured Post-Op Protocol
The post-operative phase represents your greatest opportunity to influence graft success. Our structured protocol begins with detailed written and verbal instructions covering medications, dietary modifications, oral hygiene, physical activity limitations, and specific warning signs to monitor. We provide emergency contact information for after-hours concerns, ensuring you never face complications alone.
Strategic follow-up appointments allow us to monitor healing at critical intervals – typically 24-48 hours after surgery, then at one week, two weeks, and one month. This schedule enables early intervention if complications develop. We may prescribe antimicrobial rinses, systemic antibiotics for high-risk cases, and specialized wound care products that create optimal healing conditions.
For donor site management, particularly with palatal grafts, we provide custom protective stents to prevent mechanical trauma and enhance comfort during healing. Our comprehensive approach to pain management combines appropriate medications with non-pharmacological techniques, reducing the need for extended opioid use while maintaining patient comfort.
The Recovery Timeline: What to Expect When Things Go Right
Understanding the normal healing progression helps patients distinguish between expected changes and potential problems. A typical recovery follows a relatively predictable timeline, though individual variations based on graft type, extent of recession, and patient factors are common.
Days 1-3: The Critical Window
The initial 72 hours represent the most vulnerable period for your graft. During this time, you’ll likely experience mild to moderate discomfort, some bleeding that gradually diminishes, and noticeable swelling that typically peaks around 48 hours post-surgery. The graft tissue initially appears reddish and slightly swollen, which is completely normal as inflammatory processes initiate healing.
Patients should focus on strictly following post-operative instructions during this phase – maintaining gentle pressure on any bleeding areas, taking prescribed medications on schedule, using ice packs intermittently for swelling, and avoiding all mechanical disturbance of the surgical sites. Nutrition during this period typically consists of cool, soft foods that require minimal chewing, with adequate hydration being essential for optimal healing. For more information on post-operative care, you can visit Colorado Gum Care.
Days 4-7: Early Healing Signs
By the fourth day, discomfort should begin noticeably decreasing, bleeding should have stopped completely, and swelling should begin to subside. The graft tissue starts developing a more stable appearance, though it remains fragile. The initial formation of new blood vessels (revascularization) begins during this period, though the graft still relies primarily on diffusion from surrounding tissues for survival.
Patients typically transition to a soft diet that requires minimal chewing during this phase. Prescribed antimicrobial rinses continue, but patients should still avoid brushing the surgical area. Many patients return to work or normal activities during this period, though strenuous exercise remains restricted to prevent increased blood pressure that could compromise healing.
Weeks 2-4: Progressive Integration
The second week marks significant progress in graft stability as blood vessel formation accelerates. The tissue begins appearing more pink than red, indicating improved circulation and integration with surrounding tissues. Sutures are typically removed during this period if non-resorbable materials were used, though this varies by technique and healing progress.
Most patients can gradually resume normal oral hygiene practices by the end of the second week, though with continued gentleness around the graft site. Dietary restrictions often relax at this stage, though extremely hard, crunchy, or sticky foods remain prohibited. By week three, most discomfort has resolved completely, and the graft begins resembling normal gum tissue, though complete maturation remains ongoing.
Beyond 4 Weeks: Long-Term Success Indicators
At the one-month mark, successful grafts display solid integration with surrounding tissues, natural coloration, and stable positioning. The final aesthetic results continue improving over the next several months as tissue remodeling progresses. Sensitivity reduction typically begins becoming noticeable, though complete resolution of sensitivity may take up to six months in some cases.
Complete tissue maturation takes approximately 6-12 months, during which subtle changes in texture, thickness, and appearance continue. Successful grafts maintain stable coverage of previously exposed root surfaces, with minimal recession recurrence. Ongoing monitoring at regular dental visits ensures long-term success and addresses any minor issues before they become significant problems.
If Your Graft Fails: Next Steps and Solutions
Despite best efforts, graft failures occasionally occur. When they do, understanding your options helps transform a disappointing outcome into a constructive path forward. Most importantly, graft failure doesn’t mean permanent failure – many patients achieve excellent results with alternative approaches or second attempts.
Immediate Intervention Options
When failure signs emerge early, prompt intervention can sometimes salvage the situation. If detected within the first few days, options may include additional suturing of partially detached grafts, antibiotics for developing infections, or specialized cleaning protocols for contaminated sites. The viability of these interventions depends largely on how quickly problems are identified and addressed.
In cases where salvage isn’t possible, your periodontist may recommend removing compromised tissue to prevent infection and allow the site to heal. This typically involves a simple, minimally uncomfortable procedure followed by a healing period of 4-6 weeks before considering next steps. During this interim period, temporary measures like desensitizing agents may help manage any sensitivity from re-exposed root surfaces.
Alternative Treatments to Consider
If traditional grafting proves unsuccessful, several alternative approaches deserve consideration. Guided tissue regeneration using resorbable membranes can stimulate your body’s natural healing processes to regenerate lost tissue in some cases. For patients with limited donor tissue availability, acellular dermal matrix products derived from carefully processed donor tissue offer a “scaffolding” that your body’s cells can populate.
For minor recession with primarily aesthetic concerns, pink restorative materials can sometimes provide a non-surgical solution that mimics the appearance of healthy gum tissue. Pinhole surgical technique represents another minimally invasive alternative that repositions existing tissue without grafting in selected cases. These alternatives vary in suitability depending on your specific clinical situation, tissue quality, and treatment goals.
When to Attempt a Second Graft
Many patients achieve success with a second grafting attempt, particularly when the causes of initial failure are clearly identified and addressed. Most periodontists recommend waiting at least 3-6 months after a failed graft before attempting another procedure, allowing complete healing and tissue regeneration at both donor and recipient sites. The waiting period also provides opportunity to optimize any modifiable risk factors that may have contributed to the initial failure.
Your Success Roadmap: Patient Responsibilities
While surgical technique plays a crucial role in graft success, patient cooperation during recovery exerts equally powerful influence on outcomes. Your actions during the healing period directly impact tissue integration, infection prevention, and aesthetic results. Understanding and embracing these responsibilities significantly increases your chances of achieving optimal results with minimal complications.
Critical Do’s and Don’ts After Surgery
Gum Graft Recovery Guidelines
DO apply ice packs intermittently for the first 24-48 hours
DON’T smoke or use tobacco products for at least 3 weeks
DO take all prescribed medications exactly as directed
DON’T brush or floss the surgical area until cleared by your periodontist
DO attend all scheduled follow-up appointments
DON’T exercise vigorously for at least 7 days
DO report any unusual symptoms promptly
Controlling bleeding represents an immediate priority following surgery. Apply gentle pressure with gauze pads for 20-30 minutes if bleeding occurs, and avoid vigorous rinsing, spitting, or creating suction in your mouth. These actions can dislodge blood clots that protect healing tissues and provide the foundation for graft integration.
Swelling management through intermittent ice application helps minimize tissue pressure that could compromise blood supply to the graft. Apply cold packs to the outside of your face near the surgical area for 20 minutes on, 20 minutes off during waking hours for the first 48 hours. Elevating your head while sleeping further reduces swelling by improving fluid drainage.
Oral hygiene modifications balance infection prevention with avoiding mechanical trauma. Most protocols recommend avoiding brushing and flossing near the surgical sites for 1-2 weeks, using prescribed antimicrobial rinses instead. When brushing is reintroduced, ultra-soft brushes and extremely gentle technique protect the healing graft while gradually resuming plaque control.
Dietary Modifications That Protect Your Graft
Your food choices significantly impact graft healing, particularly during the vulnerable first two weeks. Cold, soft foods predominate during the first 72 hours – yogurt, smoothies, ice cream, refrigerated soups, and similar options provide nutrition while minimizing chewing and heat exposure. As healing progresses, you can gradually incorporate lukewarm soft foods like pasta, eggs, fish, and well-cooked vegetables.
Specific foods to avoid include those that are hard, crunchy, sticky, or require significant chewing force – nuts, chips, crusty bread, tough meats, and chewy candies all pose mechanical risks to healing grafts. Extremely hot foods and beverages can increase bleeding by dilating blood vessels, while spicy foods may cause discomfort at surgical sites. Carbonated beverages, alcohol, and acidic juices should also be avoided during initial healing to prevent irritation and minimize infection risk.
Long-Term Habits for Maintaining Graft Health
Once your graft has fully healed, maintaining its long-term health requires attention to the factors that caused the initial recession. This typically includes adopting proper brushing technique (gentle, 45-degree angle, soft bristles), replacing aggressive flossing with gentler interdental cleaning methods, addressing any clenching or grinding habits through night guards if needed, and maintaining regular professional cleanings. For patients with thin tissue biotypes, ongoing vigilance with oral hygiene techniques helps prevent future recession around the grafted sites.
Frequently Asked Questions
Patients naturally have many questions about gum graft failure prevention and recovery. Here, we address the most common concerns with evidence-based, practical answers to guide you through the process with confidence and realistic expectations.
Can I smoke after a gum graft if I limit it to just one cigarette?
Even a single cigarette introduces significant risk to your healing graft. Smoking causes immediate vasoconstriction (narrowing of blood vessels) that can last for hours, dramatically reducing oxygen and nutrient delivery to the healing tissue. The chemicals in tobacco smoke also impair white blood cell function, compromising your body’s ability to prevent infection and manage the healing process.
Studies consistently show that smokers experience failure rates 2-3 times higher than non-smokers across all types of gum grafts. If you absolutely cannot abstain completely, the absolute minimum recommendation is no smoking for 48 hours before and at least two weeks after surgery, though longer abstinence significantly improves outcomes. Consider nicotine replacement options like patches (which deliver consistent low doses rather than the high-concentration spikes from cigarettes) during this critical healing period.
- Smoking causes immediate vasoconstriction lasting 30+ minutes
- Nicotine impairs fibroblast function essential for tissue repair
- Carbon monoxide reduces oxygen-carrying capacity of blood
- Harmful chemicals directly damage healing tissues
- Heat from smoking can physically damage delicate graft tissues
The bottom line: there is no “safe” level of smoking during graft healing. Your investment in the procedure deserves the maximum chance of success, which means complete tobacco avoidance during the critical healing period.
How soon can I tell if my gum graft is failing?
Most graft failures show initial warning signs within the first 7-10 days, though the timeline varies by complication type. Infection-related failures typically manifest between days 3-7 with increasing rather than decreasing pain, unusual swelling, discharge, or foul taste/odor. Blood supply issues often appear earlier, with tissue turning very white or darkening to blue/black within the first 72 hours.
Complete graft loss, where the tissue detaches entirely, can occur suddenly, while partial failures may develop more gradually over several days. This highlights the importance of both self-monitoring and attending scheduled follow-up appointments, where professional assessment can identify subtle signs of trouble before they become obvious problems. The earlier issues are detected, the more intervention options remain available.
Will insurance cover a second procedure if the first graft fails?
Insurance coverage for repeated procedures varies significantly between providers and specific plans. Most dental insurance policies that cover periodontal procedures include language regarding replacement timeframes – typically limiting coverage to one similar procedure per site within a specific timeframe (often 2-5 years). However, exceptions often exist for documented failures with clear clinical necessity for retreatment.
The key to maximizing coverage for repeated procedures lies in thorough documentation of the failure’s cause, especially when related to unforeseen complications rather than patient non-compliance. Many practices work directly with insurance companies to advocate for patients in these situations, providing the clinical documentation needed to support coverage appeals. Some periodontists also offer reduced fees for repeat procedures in cases of documented graft failure.
Are some types of gum grafts more likely to fail than others?
Different graft techniques do carry varying success rates, though patient-specific factors typically exert stronger influence on outcomes than the specific technique chosen. Pedicle grafts (which maintain their original blood supply) generally show the highest success rates at 95-98% when properly selected for appropriate cases. Connective tissue grafts follow closely at 90-95%, while free gingival grafts show slightly lower success rates at 85-90% primarily due to their complete reliance on revascularization from the recipient site.
Can medications I’m taking affect my gum graft success?
Several medication classes can significantly impact graft healing, making full disclosure to your periodontist essential. Anticoagulants and antiplatelets (including aspirin) increase bleeding risk and may interfere with stable clot formation crucial for initial graft adhesion. While these medications are rarely discontinued due to their importance for systemic health, surgical techniques can be modified to accommodate increased bleeding risk.
Immunosuppressants used for organ transplants, autoimmune conditions, or inflammatory disorders can delay healing and increase infection susceptibility. These medications typically cannot be paused, but prophylactic antibiotics and more frequent monitoring often help mitigate risks. Certain bisphosphonates used for osteoporosis deserve special consideration due to their effects on bone metabolism, though soft tissue grafting generally carries lower risk than bone-involved procedures.
Interestingly, some medications may actually benefit graft healing. Low-dose doxycycline has shown positive effects on tissue healing through matrix metalloproteinase inhibition, while certain anti-inflammatory medications may help manage tissue response when used appropriately. The key is comprehensive medication review before surgery to identify both risks and potential benefits specific to your situation.
At Coast Periodontics & Dental Implants, we’re committed to helping you achieve successful, lasting results from your gum grafting procedure through comprehensive prevention strategies and personalized care. Contact us today to learn more about our specialized approach to gum graft success.