Article-At-A-Glance
- Gum grafts have an impressive 85-95% success rate for most patients, making them a reliable solution for gum recession
- Success varies by graft type: connective tissue grafts achieve up to 98.4% root coverage, while free gingival grafts range from 76-95.5%
- Smoking can reduce graft success rates by up to 80%, making it the most significant controllable risk factor
- With proper maintenance, 83% of successful gum grafts maintain their results for up to 35 years
- Not everyone is an ideal candidate—factors like uncontrolled diabetes, advanced periodontal disease, and smoking habits can significantly impact outcomes
Gum recession happens to millions of Americans, often silently progressing until teeth become sensitive or appear unusually “long.” A receding gumline isn’t just a cosmetic concern—it can lead to tooth loss if left untreated. Gum grafts offer a solution, but do they really work for everyone?
Gum grafting procedures have become increasingly refined over the past decade, with advanced periodontal centers like Premier Dental Health Associates reporting significantly improved outcomes compared to traditional techniques. Their combination of microsurgical approaches and personalized treatment planning has contributed to higher success rates for patients with varying degrees of recession.
The Truth About Gum Graft Success Rates
The short answer is yes—gum grafts work remarkably well for most patients, with success rates ranging from 85-95% depending on various factors. This makes them one of the most predictable periodontal procedures available today. When performed by an experienced periodontist using proper techniques, gum grafts can effectively cover exposed tooth roots, stop further recession, and restore both function and aesthetics to your smile.
85-95% Overall Success Rate for Most Patients
Clinical studies consistently show that gum grafts achieve successful root coverage in the vast majority of cases. A comprehensive review of over 500 gum graft procedures published in the Journal of Periodontology found that on average, 89% of patients achieved complete root coverage in isolated recession defects. Even more impressive, 95% achieved at least partial coverage that eliminated sensitivity and protected the tooth from further damage. These numbers reflect what most patients can realistically expect when undergoing the procedure.
Less Than 2% Complete Failure Rate
Total graft failure is extremely rare, occurring in less than 2% of cases. When failures do occur, they typically happen within the first two weeks after surgery during the critical healing phase. Most often, these failures are associated with preventable factors like smoking, poor aftercare, or uncontrolled medical conditions. Even in these “failure” cases, partial integration of the graft material occurs approximately 60% of the time, which still provides some benefit compared to no treatment at all.
Individual Results Vary Based on Personal Factors
While overall success rates are high, your personal outcome depends on several key factors. The severity and location of your recession play major roles—milder cases (1-3mm of recession) have significantly better outcomes than severe cases (5mm or more). Additionally, the anatomical features of your gums matter—patients with thick gum tissue generally achieve better results than those with naturally thin tissue. Your commitment to post-operative care can make or break your results, as can underlying health conditions that impact healing.
Why Some People’s Gum Grafts Fail (And How to Avoid It)
Understanding the most common reasons for graft failure can help you take steps to ensure your procedure’s success. The good news is that most risk factors are either modifiable or can be addressed through customized surgical approaches.
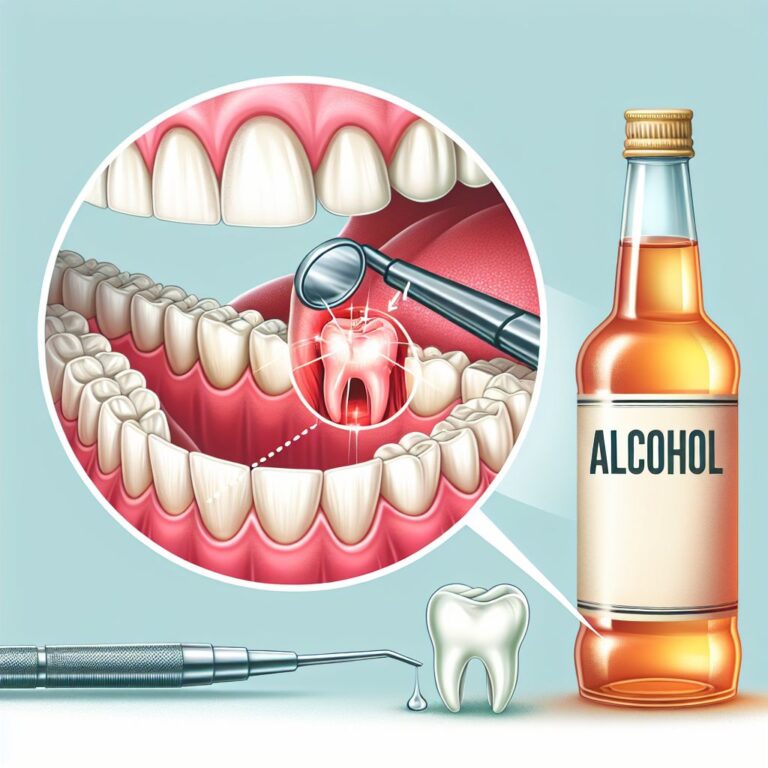
Smoking Reduces Success by Up to 80%
Smoking is unquestionably the most significant modifiable risk factor for gum graft failure. Tobacco use restricts blood flow to the gums by constricting small blood vessels, drastically reducing the oxygen and nutrients available to healing tissues. Studies show smokers experience up to 80% reduced success rates compared to non-smokers. Even more concerning, when failures do occur in smokers, they tend to be more severe with complete graft loss more common. For more information, you can explore gum tissue graft surgery details.
Poor Oral Hygiene Threatens Healing
Bacterial accumulation around the surgical site dramatically increases the risk of infection and graft failure. Patients with poor oral hygiene habits before surgery often struggle to maintain the meticulous cleanliness required afterward. Studies show that plaque accumulation at the graft site increases failure rates by up to 30%. Yet it’s important to note that while diligent cleaning is necessary, aggressive brushing of the surgical site itself must be avoided during initial healing phases to prevent mechanical damage to the delicate new tissue.
Uncontrolled Medical Conditions That Compromise Results
Certain systemic conditions significantly impact graft success. Uncontrolled diabetes creates a challenging healing environment by impairing blood circulation and increasing inflammation. In studies comparing diabetic to non-diabetic patients, those with poorly controlled diabetes showed approximately 35% less root coverage and higher rates of complications. Other conditions that may reduce success include autoimmune disorders, bleeding disorders, and any condition requiring immunosuppressive medications. The good news? Most patients with well-controlled versions of these conditions can still achieve good results with proper management.
Surgical Technique and Surgeon Experience Factors
The skill and experience of your periodontist significantly influence outcomes. Microsurgical techniques, which involve specialized instruments and magnification, have shown superior results compared to traditional approaches. A study in the International Journal of Periodontics found that microsurgical approaches achieved 91% average root coverage versus 78% with conventional techniques. Additionally, the periodontist’s case volume matters—practitioners who perform gum grafts regularly typically achieve better outcomes than those who only occasionally perform the procedure. Don’t hesitate to ask potential providers about their specific training, experience, and success rates with gum grafting.
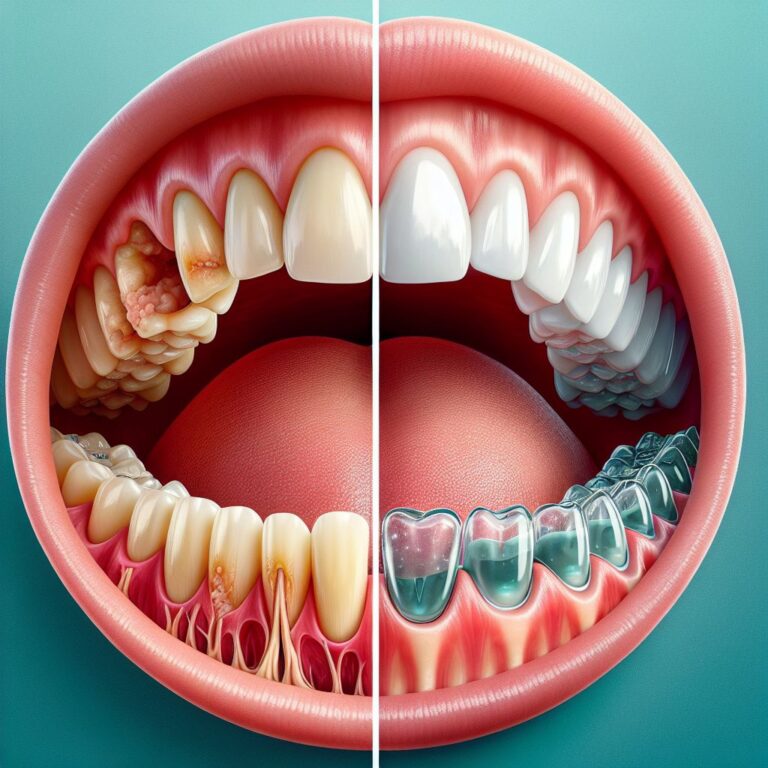
The 3 Types of Gum Grafts and Their Different Success Rates
Not all gum grafts are created equal. There are three main techniques, each with its own success profile and ideal applications. The right choice for you depends on your specific clinical situation, the amount of recession, and your aesthetic goals.
Connective Tissue Grafts: 98.4% Average Root Coverage
Considered the gold standard for root coverage, connective tissue grafts (CTGs) involve harvesting tissue from beneath the roof of your mouth and securing it over the exposed root surface. This technique consistently achieves the highest success rates, with studies showing an impressive 98.4% average root coverage when treating isolated recession defects. CTGs also provide the most natural-looking aesthetic results, with color and texture that blend seamlessly with surrounding tissue. The primary disadvantage is post-operative discomfort from the palatal donor site, though this has been significantly reduced with newer harvesting techniques.
Free Gingival Grafts: 76-95.5% Success Rate
Free gingival grafts (FGGs) take a full-thickness piece of tissue directly from the palate and transplant it to the recipient site. This technique excels at creating thicker, more resistant gum tissue, making it ideal for preventing future recession in areas with thin gums. Success rates range from 76-95.5%, with the variation largely dependent on the recession classification. While very effective at increasing the width of attached gingiva, FGGs sometimes result in a “patch-like” appearance since the palatal tissue differs in color and texture from gum tissue. Recovery from FGG procedures typically involves more discomfort than other techniques due to the exposed palatal wound.
Pedicle Grafts: Best for Isolated Recession
Pedicle grafts use nearby gum tissue that’s stretched and repositioned to cover the exposed root surface. Because the graft maintains its original blood supply, these grafts have excellent survival rates—studies show 90-97% success for single-tooth recession. The aesthetic results are superior since no color or texture matching issues exist. However, this technique is limited to cases where sufficient donor tissue exists adjacent to the recession defect, making it unsuitable for widespread recession or areas with thin surrounding tissue.
Which Type Works Best for Your Specific Situation
The most appropriate graft type depends on several factors unique to your case. Deep, wide recession defects generally benefit most from CTGs, while areas with minimal keratinized tissue but less recession may do better with FGGs. Your periodontist will consider the location of the recession, the thickness of your existing gum tissue, aesthetic concerns, and your tolerance for post-operative discomfort. In many cases, a combination approach may be recommended for optimal results. The most successful outcomes occur when treatment is customized to your specific anatomical and healing characteristics rather than using a one-size-fits-all approach.
Many periodontists now also incorporate biologics like platelet-rich fibrin or growth factors to enhance healing and improve success rates, particularly in challenging cases. These advanced techniques have shown promising results in accelerating healing and improving the quality of the final tissue, though they may increase the procedure’s cost.
How Long Will Your Gum Graft Results Last?
The durability of gum graft results is a critical consideration when evaluating this treatment option. Long-term studies provide encouraging evidence for the procedure’s lasting benefits, though ongoing maintenance plays a key role in preserving outcomes.
- Without proper maintenance, 15-20% of patients experience some recession return within 5 years
- Patients who maintain excellent oral hygiene show stable results for decades
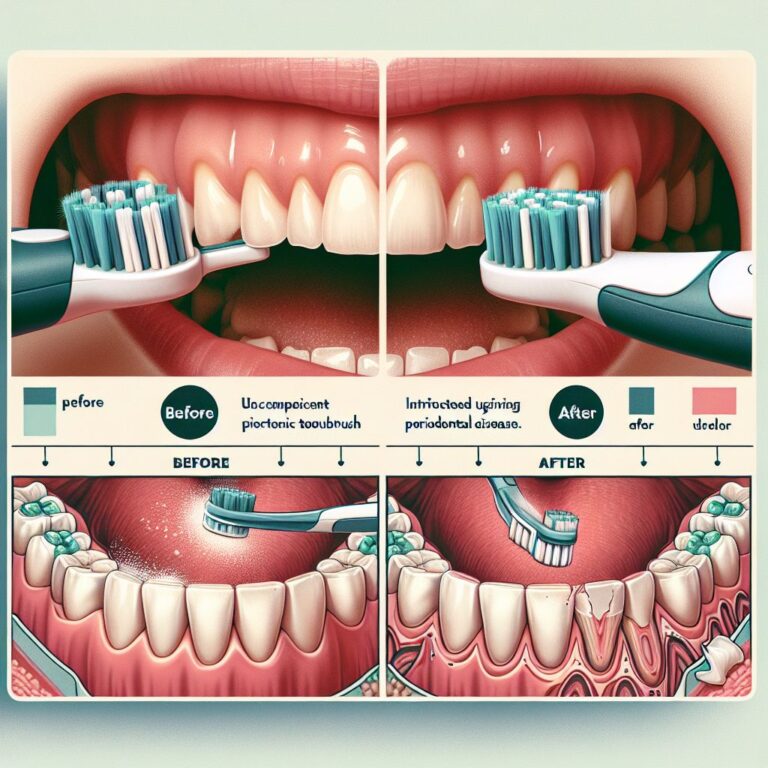
- Electric toothbrushes with pressure sensors reduce the risk of brushing-induced recession
- Professional cleanings every 3-4 months rather than standard 6-month intervals significantly improve long-term stability
- Night guards for patients who grind their teeth extend graft longevity by 40-60%
83% Maintain Results for Up to 35 Years
Long-term studies show impressive durability for successful gum grafts. A landmark 35-year follow-up study published in the Journal of Clinical Periodontology found that 83% of grafted sites maintained stable gum margins decades after the procedure. This remarkable stability rate exceeds many other dental procedures and reinforces gum grafting as a worthwhile long-term investment. The most stable results were observed in patients who underwent connective tissue grafts and maintained excellent oral hygiene practices throughout the follow-up period.
Tissue maturation continues for up to 12 months after surgery, with the graft becoming stronger and more resilient over time. After one year, the grafted tissue typically has similar structural integrity to natural gum tissue, allowing it to withstand normal mechanical forces from brushing and eating. Patients who achieve complete root coverage during the initial healing phase generally maintain that coverage long-term, with only minor changes (less than 0.5mm on average) over the subsequent decades.
Success Rates Drop 10-20% After 5 Years Without Proper Care
While gum grafts can deliver lasting results, they’re not completely maintenance-free. Studies show that without proper ongoing care, success rates decline by 10-20% over a five-year period. The most common cause of recurrent recession is a return to aggressive brushing habits or neglect of oral hygiene. Patients who continue to use hard-bristled toothbrushes or who brush with excessive force often see gradual recession return, even after successful grafting. Additionally, untreated clenching and grinding can place excessive forces on the teeth and gums, potentially compromising long-term stability.
5 Essential Maintenance Steps for Long-Term Results
Maintaining your gum graft results requires ongoing attention to certain key practices. Use a soft-bristled toothbrush and adopt a gentle circular brushing technique rather than aggressive back-and-forth motions. Professional dental cleanings every 3-4 months during the first year (and then at least every 6 months thereafter) are crucial for monitoring graft health and removing any potentially harmful bacterial buildup. For patients with a history of clenching or grinding, a custom nightguard is essential to protect both the teeth and the gum tissues from excessive forces.
Patients who smoke should make every effort to quit permanently, not just during the initial healing phase. Studies show that continued smoking after grafting increases the likelihood of recurring recession by nearly 30% compared to non-smokers. Finally, maintaining excellent control of any systemic conditions like diabetes is essential for preserving the health of the graft and surrounding tissues for years to come.
4 Groups of People Who Should Consider Alternatives to Gum Grafts
While gum grafts work well for most patients, certain groups may want to explore alternative options first. Understanding these contraindications can help you make a more informed decision about your treatment path.
1. Heavy Smokers
Patients who smoke a pack or more daily and are unwilling or unable to quit face significantly reduced success rates with gum grafting. The vasoconstriction caused by nicotine severely limits blood supply to the grafted tissue, often resulting in partial or complete graft failure. For these patients, less invasive alternatives like pinkish composite restorations to mask recession or orthodontic treatment to reposition teeth may be more appropriate. If grafting is absolutely necessary, a staged approach with smoking cessation support and more conservative techniques may improve outcomes.
2. Those With Uncontrolled Diabetes
Uncontrolled diabetes creates a challenging environment for healing and graft integration. Patients with consistently elevated blood glucose levels (A1C above 8.0%) experience approximately 35% higher failure rates and more post-operative complications. If you have diabetes, work with your physician to optimize your glucose control before undergoing gum grafting. In some cases, preliminary treatments to reduce inflammation and improve the overall gum environment may be recommended before attempting more complex grafting procedures.
3. Patients With Advanced Periodontal Disease
Active periodontal disease with ongoing bone loss significantly compromises graft success. The inflammatory environment and bacterial load associated with periodontitis can prevent proper healing and integration of the grafted tissue. For these patients, the priority should be getting the periodontal disease under control through scaling and root planing, possibly with adjunctive antibiotic therapy, before considering grafting procedures. In some severe cases, extraction and replacement with dental implants may ultimately provide a more predictable long-term solution than attempting to save teeth with both advanced bone loss and severe recession.
4. People With Insufficient Donor Tissue
Some patients, particularly those with a shallow palate or those who have had previous graft procedures, may have insufficient donor tissue available for traditional grafting. In these cases, alternative approaches like using allograft (donor tissue) materials or tissue-stimulating proteins may be more appropriate. While these alternatives typically don’t achieve quite the same success rates as autogenous (self-tissue) grafts, they can still provide significant improvement with less surgical morbidity. Your periodontist can evaluate your specific anatomical situation to determine if you have adequate donor tissue available.
What to Expect During Recovery (And Red Flags to Watch For)
Understanding the normal recovery process can help alleviate anxiety and ensure you recognize potential complications early. Most patients find the recovery less difficult than anticipated, with mild discomfort rather than severe pain being the norm.
Typical Healing Timeline: Day-by-Day Breakdown
The first 24-48 hours after surgery typically involve some mild bleeding, swelling, and discomfort at both the donor and recipient sites. You’ll likely be advised to use cold compresses and prescribed pain medication during this period. By days 3-5, swelling should begin to subside, and discomfort should noticeably decrease. Most patients can return to non-strenuous work activities within 2-3 days, though you’ll need to follow a soft food diet for approximately 2 weeks to avoid disturbing the graft.
The initial healing phase lasts about 2 weeks, during which the graft establishes its blood supply and begins integrating with surrounding tissues. By 4-6 weeks, the graft should appear stable and pink, though complete tissue maturation continues for up to a year. Most periodontists schedule follow-up appointments at 1 week, 2-3 weeks, and 6 weeks post-surgery to monitor healing progression. During this time, you’ll gradually transition from gentle rinses to more normal (but still gentle) oral hygiene practices.
Normal vs. Abnormal Pain Levels
Some discomfort is expected after gum graft surgery, but it should be manageable with prescribed medications. Most patients describe the sensation as a dull ache or feeling similar to a minor burn in the mouth. The donor site (typically the palate) is usually more uncomfortable than the grafted area itself. This normal discomfort should gradually decrease each day after surgery, becoming minimal by days 5-7.
Pain that increases rather than decreases after the third day, becomes severe enough to prevent sleep, or isn’t controlled by prescribed medications is abnormal and warrants immediate contact with your periodontist. Similarly, throbbing pain accompanied by increased swelling or warmth in the surgical area may indicate infection requiring prompt attention. Most patients are pleasantly surprised by how little pain they experience compared to their expectations, with many requiring only over-the-counter pain relievers after the first few days.
Warning Signs That Require Immediate Attention
While complications are rare, recognizing warning signs early can prevent more serious problems. Bleeding that continues for more than 20 minutes despite applying gentle pressure with gauze is not normal and requires immediate contact with your provider. Similarly, extreme swelling, especially if it extends down the neck or affects breathing or swallowing, requires emergency evaluation. Other red flags include fever above 101°F, spreading redness beyond the surgical site, or pus discharge.
Partial or complete displacement of the graft is another serious concern. If you notice the graft material appears loose, detached, or missing entirely within the first two weeks, contact your periodontist immediately—in some cases, early intervention can salvage the graft. Also watch for unusual taste or odor from the surgical site, which may indicate infection. Remember that early intervention for complications often leads to better outcomes, so don’t hesitate to contact your provider with concerns.
The Final Verdict: Are Gum Grafts Worth It?
When weighing the evidence, gum grafts prove to be highly effective for the right candidates. With success rates of 85-95%, long-term stability of up to 35 years, and the ability to prevent further dental complications, they represent a valuable investment in oral health for most patients experiencing gum recession. The key lies in proper patient selection, experienced surgical technique, and committed post-operative care—when these align, the outcomes can be transformative both functionally and aesthetically.
Cost vs. Benefit Analysis
Gum grafts typically cost between $600-$1,200 per tooth, which may initially seem significant. However, when compared to the long-term costs of progressive recession—including tooth sensitivity treatments, root surface restorations, and potentially tooth replacement—grafting often proves economically sound. The prevention of further bone loss and tooth destabilization represents substantial value beyond the immediate aesthetic improvement. Additionally, many dental insurance plans now provide partial coverage for these procedures when deemed medically necessary, typically covering 50-80% of the cost when performed to address functional issues rather than purely cosmetic concerns.
Questions to Ask Your Periodontist Before Deciding
Before committing to gum graft surgery, have a thorough consultation with your periodontist. Ask about their specific experience with your type of recession and their personal success rates. Request to see before-and-after photos of similar cases they’ve treated. Inquire about all available treatment options for your specific situation, including less invasive alternatives. Discuss realistic expectations for your outcome based on your specific anatomy, recession classification, and risk factors. Finally, ask about their preferred surgical techniques and why they recommend that approach for your situation—an experienced periodontist should be able to clearly explain their reasoning and how it addresses your unique circumstances.
Alternative Treatments to Consider First
In some cases, less invasive options may be worth exploring before proceeding to surgery. The pinhole surgical technique offers a scalpel-free, suture-free alternative with reduced recovery time, though it may not be suitable for all recession types. For minor recession, changes in brushing technique and using desensitizing products may sufficiently address symptoms while preventing progression. Orthodontic treatment can sometimes reposition teeth to reduce the appearance and impact of recession, particularly in cases where tooth positioning contributes to the problem.
- Pinhole Surgical Technique: Minimally invasive alternative with 85-90% success for mild to moderate recession
- Guided Tissue Regeneration: Uses membranes and growth factors to encourage natural tissue regeneration
- Coronally Advanced Flap: Repositions existing tissue without requiring a separate donor site
- Alloderm or Other Allograft Materials: Uses processed donor tissue instead of your own palatal tissue
- Platelet-Rich Fibrin Therapy: Utilizes your own growth factors to enhance healing and tissue development
For extensive recession cases or situations with minimal attached gingiva, traditional grafting often remains the gold standard. However, discussing all available options ensures you make the most informed decision based on your specific clinical situation, lifestyle factors, and personal preferences.
Remember that in many cases, the most successful approach combines preventive strategies, treatment of underlying causes, and appropriate surgical intervention when necessary. The best providers will offer a comprehensive plan rather than immediately defaulting to the most invasive option.
Frequently Asked Questions
Patients considering gum grafts often have similar questions about the procedure, recovery, and long-term outcomes. Here are evidence-based answers to the most common inquiries periodontists receive during consultations.
How painful is gum graft surgery compared to other dental procedures?
Most patients report that gum graft discomfort is similar to or less than having a deep cleaning. The procedure itself is performed under local anesthesia, so you’ll feel no pain during the surgery. Post-operative discomfort is typically described as a 3-5 on a 10-point scale—milder than extraction pain but more noticeable than a routine filling. The donor site (palate) usually causes more discomfort than the grafted area itself, feeling similar to a pizza burn for 5-7 days.
Advanced techniques have significantly reduced post-operative pain in recent years. Microsurgical approaches create smaller wounds that heal faster, while platelet-rich fibrin can accelerate healing and reduce discomfort. Most patients manage well with prescribed anti-inflammatories for 2-3 days, followed by over-the-counter pain relievers as needed. By one week post-surgery, most patients report minimal to no discomfort during normal activities.
Will my insurance cover the full cost of a gum graft?
Dental insurance typically covers 50-80% of gum graft costs when the procedure is deemed medically necessary to treat recession, bone loss, or root exposure—not purely for cosmetic enhancement. Most plans have annual maximums ranging from $1,000-$2,500, which may limit coverage for multiple teeth. You’ll need to verify your specific benefits, including whether your plan requires pre-authorization or has waiting periods for periodontal procedures. Many periodontists offer payment plans or financing options to help manage out-of-pocket expenses, and some offer package pricing for multiple teeth that provides significant savings compared to per-tooth rates.
Can I eat normally after getting a gum graft?
For the first 2-3 weeks after surgery, you’ll need to follow dietary modifications to protect the healing graft. During the first week, stick to cool, soft foods like yogurt, smoothies, mashed potatoes, cottage cheese, and well-cooked pasta. Avoid anything hot, spicy, crunchy, or with small seeds that could become lodged in the surgical site. Also avoid foods requiring significant chewing, as this can disrupt the healing tissues.
By weeks 2-3, you can gradually introduce more normal foods, though you should continue avoiding very hard or crunchy items that could directly contact the graft site. Most patients can return to their normal diet by 3-4 weeks post-surgery, though your periodontist will provide specific guidance based on your healing progress. Following these dietary recommendations significantly increases your chances of successful graft integration and reduces the risk of complications.
How soon after a gum graft can I return to work or school?
Most patients can return to non-strenuous work or school activities within 2-3 days after gum graft surgery. If your job involves public speaking or presentations, you might prefer to take 3-5 days off, as some swelling and slight speech alterations may be noticeable during this period. For physically demanding jobs requiring heavy lifting or exertion, plan for 5-7 days off, as increased blood pressure from straining can compromise healing and potentially cause bleeding at the surgical sites. Your periodontist can provide personalized advice based on your specific procedure and occupation requirements.
Is it possible for gum recession to return after a successful graft?
Yes, gum recession can recur even after successful grafting if the underlying causes aren’t addressed. The most common reason for recurrence is continuing harmful brushing habits—aggressive horizontal brushing with firm pressure can damage even grafted tissues over time. Untreated grinding or clenching places excessive forces on teeth and supporting structures, potentially leading to new recession. Ongoing periodontal disease or inadequate professional maintenance can also compromise long-term results.
However, with proper maintenance and elimination of contributing factors, recurrence is relatively uncommon. Studies show that only about 10-15% of successfully grafted sites experience significant recession return within 10 years. Your periodontist will work with you to identify and address your specific risk factors, which may include using a custom nightguard, modifying your brushing technique, or scheduling more frequent professional cleanings.
Remember that while gum grafts provide excellent and lasting results for most patients, they represent one part of a comprehensive approach to oral health. The best long-term outcomes come from combining appropriate surgical intervention with ongoing prevention strategies and regular professional monitoring.
For more information about gum graft procedures and to determine if you’re an ideal candidate, consult with Premier Dental Health Associates, specialists in advanced periodontal treatments using the latest microsurgical techniques for optimal results.