Key Takeaways: Mastic Gum’s Evidence-Based Benefits
- Mastic gum has shown significant promise in fighting H. pylori infections, the bacteria responsible for many stomach ulcers, with clinical studies supporting its effectiveness.
- Research demonstrates mastic gum’s antibacterial properties benefit oral health by reducing plaque formation and fighting bacteria that cause gum disease.
- Clinical trials have found that mastic gum supplementation may help improve cholesterol profiles and regulate blood glucose levels.
- While some anti-inflammatory properties have been observed in laboratory studies, real-world clinical evidence is still developing for conditions like IBD and IBS.
- Quality matters—authentic mastic gum comes specifically from the island of Chios in Greece and its effectiveness depends on proper dosing and consistent use.
What Is Mastic Gum? The Ancient Healing Resin Making a Comeback
Mastic gum is a resinous substance harvested from the trunk and branches of the mastic tree (Pistacia lentiscus var. Chia) that grows predominantly on the Greek island of Chios. This aromatic, crystalline resin has been used medicinally for thousands of years across Mediterranean and Middle Eastern cultures. Ancient Greek physicians like Hippocrates documented its use for digestive ailments and respiratory conditions, while Romans chewed it as one of the world’s first natural chewing gums.
The harvesting process remains largely unchanged since ancient times—small incisions are made in the bark during summer months, allowing the resin to drip and harden into yellowish-white “tears” that are collected by hand. What makes this substance special is its unique composition of over 70 natural compounds including essential oils, antioxidants, and terpenes. These bioactive components are responsible for mastic gum’s therapeutic properties that modern research has begun to scientifically validate.
Today, mastic gum is experiencing a renaissance in natural medicine circles, available in various forms including raw tears for chewing, powders, capsules, and tinctures. Its recent popularity stems from growing scientific evidence supporting what traditional healers knew centuries ago—this resin offers numerous health benefits, particularly for digestive health, oral care, and inflammation reduction.
Digestive Relief: The Most Proven Benefit of Mastic Gum
Digestive health represents the most extensively studied and validated area of mastic gum’s therapeutic potential. Traditional use for stomach ailments has now been backed by multiple clinical trials showing significant benefits for various gastrointestinal issues. The resin’s natural compounds appear to create an environment in the digestive tract that’s inhospitable to harmful bacteria while soothing irritated tissues.
Several studies have demonstrated that regular consumption of mastic gum can reduce stomach pain, bloating, and general digestive discomfort. A randomized, placebo-controlled trial published in the Journal of Ethnopharmacology found that patients with functional dyspepsia (persistent upper abdominal pain or discomfort) experienced significant symptom improvement after taking mastic gum supplements for three weeks compared to those taking placebo.
How Mastic Gum Fights H. pylori Infections
Perhaps the most impressive digestive benefit of mastic gum is its ability to combat Helicobacter pylori, the bacteria responsible for most stomach ulcers and many cases of chronic gastritis. This discovery was first published in the New England Journal of Medicine in 1998, bringing scientific validation to a traditional remedy. The study found that even low doses of mastic gum could kill H. pylori in the laboratory setting.
Following this breakthrough, a clinical trial published in Phytomedicine in 2010 confirmed these effects in humans. Researchers found that mastic gum supplements taken for two weeks significantly reduced H. pylori bacterial load in patients with diagnosed infections. Nearly 30% of participants experienced complete eradication of the bacteria—a remarkable result for a natural substance. The mechanism appears to involve disruption of bacterial cell membranes and inhibition of bacterial adhesion to stomach tissue.
What makes mastic gum particularly valuable is its gentle action compared to conventional antibiotics often prescribed for H. pylori. While antibiotics can disrupt the entire gut microbiome, causing side effects like diarrhea and yeast overgrowth, mastic gum appears to target harmful bacteria more selectively. This makes it an appealing option either as a complementary approach alongside conventional treatment or as a preventative measure for those at risk of recurrent infections.
Clinical Evidence for Reducing Stomach Pain and Indigestion
Beyond its antibacterial properties, mastic gum demonstrates broader benefits for digestive comfort. Clinical research has shown its effectiveness in treating functional dyspepsia, a common condition characterized by chronic stomach pain, bloating, early satiety, and nausea without identifiable organic cause. A randomized controlled trial involving 148 patients found that those taking mastic gum experienced significant improvement in overall symptom scores compared to placebo groups.
The resin appears to work through multiple mechanisms to provide digestive relief. Its mild anti-inflammatory properties help soothe irritated stomach lining, while its ability to regulate gastric acid secretion creates a more balanced digestive environment. Additionally, mastic gum contains compounds that promote healthy bile flow, potentially improving fat digestion and reducing related discomfort.
Potential Benefits for IBS and IBD Sufferers
Emerging research suggests mastic gum may offer relief for those suffering from inflammatory bowel conditions like irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). The resin’s anti-inflammatory properties appear particularly beneficial for calming the chronic inflammation that characterizes these conditions. While large-scale clinical trials are still needed, preliminary studies and anecdotal evidence from practitioners indicate potential for symptom management.
For IBS sufferers, mastic gum may help regulate bowel movements and reduce abdominal pain by calming intestinal spasms. The resin’s mild antimicrobial effects could also help address potential bacterial imbalances that often accompany IBS. For IBD patients, including those with Crohn’s disease and ulcerative colitis, mastic gum’s documented ability to reduce inflammatory markers suggests it might help manage flare-ups when used as a complementary approach alongside conventional treatments.
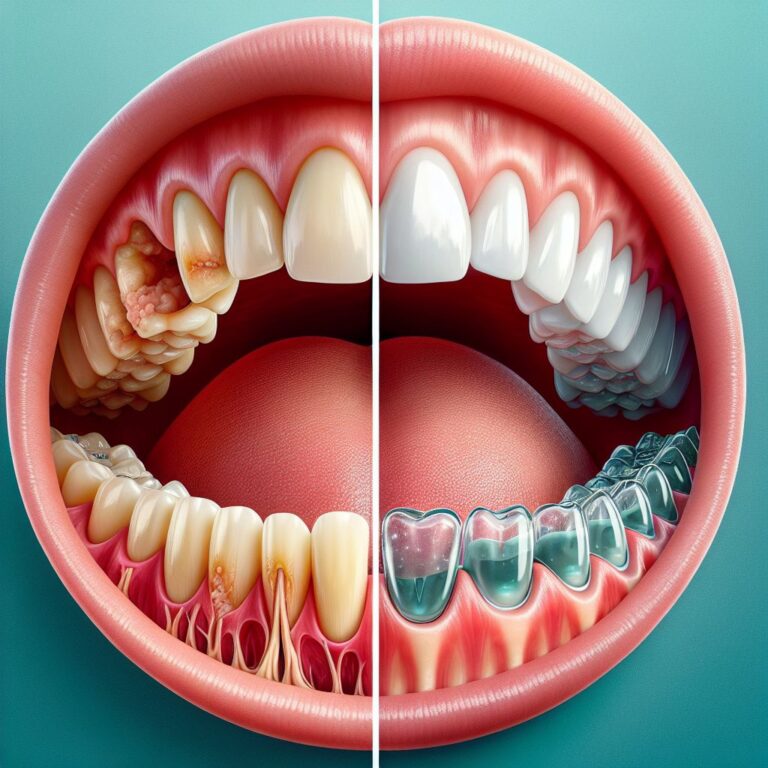
Oral Health Benefits You Can Actually Count On
Long before modern dental care, mastic gum served as nature’s toothbrush throughout the Mediterranean. This traditional use has strong scientific backing, with multiple studies confirming mastic gum’s significant benefits for oral health. The resin contains natural compounds that specifically target bacteria responsible for dental plaque, cavities, and gum disease.
Regular mastic gum chewing creates a mechanical cleaning action while releasing antibacterial compounds directly into the oral cavity. These compounds can reach areas that brushing might miss, providing comprehensive protection against oral pathogens. Additionally, mastic gum stimulates saliva production, which helps neutralize acids and remineralize tooth enamel, further protecting against decay.
Bacteria-Fighting Properties That Reduce Plaque
Clinical research has demonstrated mastic gum’s remarkable ability to combat oral bacteria, particularly those responsible for plaque formation. A study published in the Journal of Periodontology found that mastic gum extract significantly reduced the growth of Streptococcus mutans and Porphyromonas gingivalis, two primary bacterial culprits in dental disease. The resin’s compounds appear to disrupt bacterial cell walls and interfere with their ability to adhere to tooth surfaces.
What makes mastic gum particularly valuable is its selective antimicrobial action. Unlike chemical mouthwashes that can disrupt the entire oral microbiome, mastic gum appears to primarily target harmful bacteria while preserving beneficial ones. This balanced approach supports overall oral ecosystem health rather than creating a sterile environment that can lead to opportunistic infections.
In practical application, studies comparing plaque levels between mastic gum users and non-users show significant reductions in plaque formation after just two weeks of regular use. This makes it an excellent complement to standard oral hygiene practices, particularly for those prone to rapid plaque buildup despite diligent brushing and flossing.
Protection Against Gum Disease and Cavities
Beyond plaque reduction, mastic gum offers specific benefits for preventing more serious dental conditions. Clinical research indicates the resin can reduce gingival inflammation markers and bleeding during dental probing, two early indicators of periodontal disease. These anti-inflammatory effects stem from compounds that inhibit prostaglandin production in gum tissue, calming the inflammatory response that leads to gum recession and bone loss.
For cavity prevention, mastic gum works through multiple mechanisms. Its antibacterial action reduces acid-producing bacteria, while its ability to stimulate saliva flow helps neutralize acids that erode enamel. Additionally, some studies suggest mastic gum components may actually strengthen tooth enamel through remineralization, creating more resistance to acid attack.
How Long to Chew for Maximum Benefits
To obtain maximum oral health benefits from mastic gum, research suggests an optimal chewing duration of 15-20 minutes at least twice daily. This timing allows for complete release of the resin’s bioactive compounds while providing sufficient mechanical cleaning action. Studies indicate that benefits begin appearing after approximately two weeks of consistent use, with more significant improvements observed after 4-6 weeks.
The timing of mastic gum chewing also matters. For best results, dental researchers recommend chewing after meals when bacterial activity is highest and saliva production is needed most to neutralize acids. This post-meal chewing habit can significantly reduce the risk of cavity formation during the critical 30-60 minute window following food consumption when enamel is most vulnerable to acid attack.
Cholesterol and Heart Health: What the Research Shows
Beyond digestive and oral benefits, mastic gum shows promising effects on cardiovascular health markers, particularly cholesterol profiles. This potential benefit has been the subject of several clinical trials with encouraging results. The resin appears to influence lipid metabolism through multiple pathways, offering a natural approach to supporting heart health.
The connection between mastic gum and cholesterol management isn’t merely coincidental. Research has identified specific compounds in the resin that interact with peroxisome proliferator-activated receptors (PPARs), important regulators of lipid and glucose metabolism. These interactions may explain mastic gum’s observed effects on cholesterol levels and provide a scientific basis for its traditional use in supporting cardiovascular health.
Promising Results from Human Studies
A pivotal clinical trial published in the European Journal of Preventive Cardiology examined mastic gum’s effects on healthy volunteers with normal to mildly elevated cholesterol levels. After 8 weeks of daily supplementation, participants showed significant reductions in total cholesterol and LDL (bad) cholesterol compared to the placebo group. Importantly, beneficial HDL cholesterol levels remained stable or slightly increased, indicating a balanced effect on lipid profiles.
Another notable study published in the Journal of Medicinal Food found that mastic gum supplementation not only improved cholesterol levels but also reduced markers of oxidative stress in participants. This dual action is particularly valuable since oxidized LDL cholesterol plays a key role in atherosclerosis development. By both reducing LDL levels and protecting against oxidation, mastic gum addresses two critical factors in cardiovascular disease progression.
Beyond cholesterol effects, research indicates mastic gum may help regulate blood glucose levels, another important factor in heart health. A randomized controlled trial found that participants taking mastic gum supplements experienced modest but significant improvements in fasting glucose levels compared to placebo groups. This glucose-regulating effect may be particularly beneficial for those with metabolic syndrome or pre-diabetic conditions that increase cardiovascular risk.
Recommended Dosage for Cholesterol Support
For those seeking to improve cholesterol profiles with mastic gum, clinical research suggests specific dosing protocols for optimal results. Most successful studies used daily doses ranging from 1-3 grams, typically divided into multiple administrations throughout the day. This divided approach appears to maintain more consistent levels of active compounds in the bloodstream, enhancing their regulatory effects on lipid metabolism.
The form of mastic gum may influence effectiveness for cholesterol management. Encapsulated supplements often provide more precise dosing than chewing the raw resin, though both methods show benefit. Some practitioners recommend taking mastic gum supplements with meals containing healthy fats, as this may enhance absorption of the resin’s fat-soluble compounds. For most individuals, noticeable improvements in lipid profiles typically emerge after 8-12 weeks of consistent use, though this timeline varies based on individual metabolism and concurrent lifestyle factors.
Anti-Inflammatory Properties: Separating Hope from Hype
Mastic gum’s anti-inflammatory capabilities represent one of its most promising yet complex areas of therapeutic potential. Laboratory studies consistently demonstrate the resin’s ability to reduce inflammatory markers and modulate immune responses. These properties stem from several compounds that inhibit pro-inflammatory cytokines and enzymes involved in the inflammatory cascade.
However, translating these laboratory findings to clinical applications requires careful consideration. While cell and animal studies show clear anti-inflammatory effects, human clinical trials have yielded more variable results. The strongest evidence exists for localized anti-inflammatory benefits in the digestive tract and oral cavity, where the resin makes direct contact with tissues. Systemic anti-inflammatory effects throughout the body, while biologically plausible, have less robust clinical documentation.
This distinction between laboratory promise and clinical reality doesn’t diminish mastic gum’s value but rather helps establish realistic expectations. The resin likely offers meaningful anti-inflammatory support, particularly for conditions involving the digestive system, but should be viewed as a complementary approach rather than a primary treatment for serious inflammatory disorders.
Laboratory Evidence vs. Clinical Reality
The laboratory evidence for mastic gum’s anti-inflammatory properties is compelling. In vitro studies show that mastic gum extracts inhibit production of inflammatory mediators like tumor necrosis factor-alpha (TNF-α) and interleukins. These compounds play key roles in triggering and sustaining inflammatory responses throughout the body. Additionally, mastic gum components demonstrate antioxidant effects that further support tissue protection during inflammatory processes.
Translating these laboratory findings to human benefits, however, involves several challenges. Bioavailability—how well these compounds are absorbed and reach target tissues—represents a significant consideration. Some of mastic gum’s anti-inflammatory compounds may have limited absorption or undergo substantial metabolism before reaching systemic circulation. This may explain why direct contact applications (like chewing for oral inflammation or ingesting for digestive tract inflammation) show more consistent benefits than those requiring systemic distribution.
Clinical studies examining inflammatory markers in humans taking mastic gum supplements show more variable results than laboratory predictions would suggest. While some participants experience significant reductions in inflammatory biomarkers like C-reactive protein (CRP), others show minimal changes. This variability likely reflects differences in individual metabolism, concurrent inflammation drivers, and genetic factors that influence response to plant compounds.
Conditions That May Respond to Mastic Gum
Despite the nuances in translating laboratory findings to clinical applications, several inflammatory conditions show particular promise for mastic gum intervention. Inflammatory bowel conditions including Crohn’s disease and ulcerative colitis have demonstrated positive responses in preliminary studies, likely due to direct contact between the resin’s compounds and inflamed intestinal tissues. Similarly, inflammatory dental conditions like gingivitis and periodontitis respond well to mastic gum’s local anti-inflammatory effects.
Emerging research suggests potential benefits for inflammatory skin conditions when mastic gum is applied topically. Traditional Mediterranean healing practices have long used mastic preparations for wound healing and skin inflammation, and modern research has begun validating these applications. Laboratory studies show mastic extracts can reduce inflammatory markers in skin cells and promote healing processes, though larger clinical trials are still needed.
For systemic inflammatory conditions like rheumatoid arthritis and metabolic inflammation, the evidence remains preliminary. While some individuals report subjective improvements, controlled clinical trials show more modest effects than local applications. These conditions may still benefit from mastic gum’s general anti-inflammatory properties, but expectations should be calibrated accordingly. For more detailed insights, you can refer to this clinical trial study.
Popular Myths About Mastic Gum You Shouldn’t Believe
As with many traditional remedies gaining modern attention, mastic gum has accumulated several exaggerated or unfounded claims. Distinguishing between evidence-based benefits and marketing hype helps consumers make informed decisions and maintain realistic expectations. Some popular misconceptions have emerged that deserve critical examination.
The internet abounds with testimonials suggesting mastic gum can treat dozens of conditions without scientific substantiation. While the resin offers legitimate health benefits, approaching claims with healthy skepticism protects consumers from disappointment and potential health risks from neglecting proven treatments. Understanding both the real benefits and limitations of mastic gum allows for its appropriate integration into health practices.
Perhaps most importantly, recognizing that quality research on mastic gum continues to evolve prevents both premature dismissal and overenthusiastic adoption. The resin offers genuine therapeutic potential supported by centuries of traditional use and growing scientific validation, but responsible use requires distinguishing between established benefits and areas still requiring research confirmation.
The “Miracle Cure” Misconception
Among the most problematic myths surrounding mastic gum is its portrayal as a “miracle cure” for serious medical conditions. While the resin demonstrates legitimate therapeutic properties, claims of curing cancer, reversing heart disease, or eliminating autoimmune disorders lack scientific support. These exaggerated claims potentially harm consumers by delaying proven medical interventions or creating false hope.
The reality is that mastic gum offers modest but meaningful benefits for specific conditions, particularly those involving digestive health, oral health, and certain inflammatory processes. These benefits derive from well-studied biological mechanisms rather than miraculous properties. Understanding mastic gum as one beneficial component within a comprehensive health approach—rather than a panacea—allows for its appropriate integration into wellness practices.
Weight Loss Claims: What Science Actually Says
Another common misconception surrounds mastic gum’s purported weight loss benefits. While some products market the resin as a weight loss aid, scientific evidence for this specific application remains limited. The confusion likely stems from mastic gum’s ability to improve digestive function and potentially reduce bloating, which might create a subjective feeling of weight change without affecting actual fat loss.
The modest glucose-regulating effects observed in some studies might theoretically support metabolic health, which indirectly relates to weight management. However, no well-designed clinical trials have demonstrated significant weight loss effects from mastic gum supplementation alone. Those seeking weight management support should view mastic gum as a minor complementary approach at best, while focusing primarily on established strategies like balanced nutrition and regular physical activity.
False Expectations About Cancer Prevention
Perhaps the most concerning myths involve claims about mastic gum’s cancer-fighting properties. While laboratory studies have indeed shown that certain compounds in mastic gum can induce apoptosis (programmed cell death) in cancer cell lines, these findings represent very preliminary research conducted outside living organisms. The significant leap from laboratory observations to cancer prevention or treatment in humans remains unsupported by clinical evidence.
Laboratory studies examining isolated compounds in artificial environments cannot predict how these substances will behave in the complex human body with its various metabolic processes, absorption barriers, and protective mechanisms. Additionally, many natural compounds show anti-cancer effects in laboratory settings without translating to clinical benefits. While mastic gum may contain compounds worthy of continued cancer research, current evidence doesn’t support its use for cancer prevention or treatment.
How to Choose Quality Mastic Gum Products
With growing popularity comes increasing market diversity, making product selection increasingly challenging. Quality varies dramatically among mastic gum products, with significant implications for both effectiveness and safety. Understanding key quality indicators helps consumers make informed choices that maximize potential benefits while minimizing risks.
Three primary factors determine mastic gum quality: authenticity of source, processing methods, and additional ingredients. These factors influence not only the concentration of beneficial compounds but also potential contamination risks. Learning to evaluate products based on these criteria empowers consumers to identify truly beneficial options among marketing claims.
The Importance of Chios Origin
Authentic mastic gum comes specifically from the Greek island of Chios, where unique environmental conditions create the highest concentration of beneficial compounds in the resin. The Pistacia lentiscus var. Chia trees growing on this island produce resin with demonstrably different chemical profiles than related trees elsewhere. This difference stems from the island’s particular soil composition, climate, and the specific genetic variety of trees cultivated there for centuries.
Mastic gum from Chios has been granted Protected Designation of Origin (PDO) status by the European Union, recognizing its unique properties and historical significance. Products using authentic Chios mastic typically indicate this origin on packaging, often with certification from the Chios Mastiha Growers Association. This certification provides assurance of authenticity and adherence to traditional harvesting and processing methods that preserve beneficial compounds.
While some products may contain resins from related Pistacia species or non-Chios sources, these alternatives lack the specific compound profile that research has associated with therapeutic benefits. The price premium for authentic Chios mastic reflects not only limited supply but also meaningfully different composition that directly impacts effectiveness.
Forms Available: Tears, Powder, Capsules and Gum
Mastic gum comes in several forms, each offering different advantages for specific health goals. The most traditional form—whole “tears” or crystals—provides the purest experience but requires direct chewing. These natural tears offer maximum potency for oral health benefits and traditional digestive uses, though some find their initial bitter taste challenging before it develops into a pleasant pine-like flavor.
Powdered mastic provides greater versatility, allowing incorporation into foods, beverages, or homemade remedies. This form offers good bioavailability while enabling precise dosing for specific health applications. However, powdered products vary significantly in purity and processing methods, with some losing volatile compounds during production.
Encapsulated supplements offer convenience and precise dosing for specific health goals like H. pylori management or cholesterol support. Quality capsule products should specify exact mastic content (typically 250-1000mg per capsule) and ideally include information about the resin’s origin. Some supplements combine mastic with complementary ingredients like DGL licorice or zinc for digestive applications, potentially enhancing specific benefits.
- Tears/Crystals: Best for oral health, traditional chewing, highest purity
- Powder: Most versatile for culinary and custom applications
- Capsules: Most convenient for specific health goals requiring precise dosing
- Commercial chewing gum: Variable mastic content, often contains additional sweeteners and ingredients
Price Points: Why Cheap Isn’t Always Better
Authentic mastic gum commands premium prices reflecting its limited production, labor-intensive harvesting, and the specialized knowledge required for proper collection and processing. The entire world’s annual production of Chios mastic amounts to only about 200 tons, with demand consistently exceeding supply. This limited availability creates economic pressure that unfortunately encourages counterfeit or adulterated products.
Products offering mastic gum at surprisingly low prices often contain minimal amounts of actual resin, diluted with cheaper substitutes like other tree resins or synthetic compounds. These adulterations not only reduce effectiveness but potentially introduce unwanted substances. Realistic price expectations for quality products include approximately $15-25 for 10 grams of pure tears, $20-40 for a month’s supply of capsules, and proportionally higher prices for concentrated extracts.
Proper Usage Guide: Getting the Most from Mastic Gum
Maximizing mastic gum’s benefits requires understanding proper administration methods, timing, and duration of use. Different health applications demand different approaches to optimize results while minimizing potential side effects. Strategic use based on therapeutic goals ensures the best outcomes from this versatile natural remedy.
Beyond basic dosing guidelines, factors like timing relative to meals, consistency of use, and complementary lifestyle practices significantly influence results. Additionally, realistic timelines for expected benefits help maintain motivation for continued use, as many of mastic gum’s effects develop gradually rather than immediately.
Effective Dosages Based on Your Health Goals
Clinical research suggests specific dosage ranges for different health applications, with significant variation based on the targeted benefit. For H. pylori management and general digestive support, studies typically use 1-2 grams daily, divided into multiple doses. This moderate dosage demonstrates good effectiveness while minimizing potential digestive adjustment periods that can occur with higher amounts.
For cholesterol and metabolic support, slightly higher dosages of 2-3 grams daily show the most consistent benefits in clinical trials. This increased amount may be necessary to achieve systemic effects beyond the digestive tract. For oral health applications, the mechanical action of chewing becomes relevant alongside chemical properties, with recommendations for chewing approximately 1 gram (a small tear) for 15-20 minutes after meals.
Regardless of health goal, starting with lower dosages and gradually increasing allows the body to adjust and helps identify individual tolerance thresholds. Some people experience mild digestive adaptation symptoms when first taking mastic gum, including temporary changes in bowel movements or mild abdominal sensations that typically resolve within a few days of consistent use.
Best Times to Take Mastic Gum
Timing mastic gum consumption strategically enhances its effectiveness for specific health goals. For digestive applications, particularly H. pylori management, taking mastic on an empty stomach 30 minutes before meals provides direct contact with gastric tissues before food interference. This timing maximizes the resin’s interaction with gastric mucosa and potential pathogens while minimizing dilution by food and digestive secretions.
How Long Before You See Results
Expectation management regarding timeframes for observable benefits helps prevent premature discontinuation of potentially beneficial regimens. For digestive applications, particularly symptom relief from functional dyspepsia or mild gastritis, many users report noticeable improvements within 1-2 weeks of consistent use. However, more significant goals like H. pylori reduction typically require at least 4-6 weeks of regular administration, with some studies suggesting optimal results after 8-12 weeks.
Cholesterol and metabolic benefits generally emerge more gradually, with measurable changes in lipid profiles typically requiring 8-12 weeks of consistent supplementation. These effects often continue improving with longer-term use, suggesting cumulative benefits from consistent administration. Oral health applications may show more rapid results, with noticeable reductions in plaque formation and gingival inflammation often apparent within 2-3 weeks of regular use.
- Digestive symptom relief: 1-2 weeks for initial improvements
- H. pylori reduction: 4-12 weeks for significant effects
- Cholesterol improvements: 8-12 weeks for measurable changes
- Oral health benefits: 2-3 weeks for noticeable effects
Individual response variations stem from factors including baseline health status, concurrent dietary patterns, genetic factors affecting metabolism of plant compounds, and overall inflammatory burden. Those with more significant health challenges may require longer treatment durations, while those using mastic preventatively or for minor issues often experience faster results.
Who Should Avoid Mastic Gum: Safety Considerations
While mastic gum demonstrates an excellent safety profile for most individuals, certain populations should exercise caution or avoid use entirely. Understanding these contraindications helps prevent adverse reactions and ensures appropriate use of this natural remedy. Safety considerations include both absolute contraindications and situations requiring professional guidance.
As with any bioactive substance, individual variations in metabolism, pre-existing conditions, and concurrent medications can influence safety and appropriate use. These variations highlight the importance of personalized approaches to natural remedies rather than universal recommendations. Consulting healthcare providers before beginning mastic gum supplementation represents a prudent approach, particularly for those with complex health situations.
Despite these considerations, mastic gum’s overall safety record remains impressive, with few documented adverse effects in thousands of years of traditional use and numerous clinical trials. Most reported side effects are mild and transient, primarily involving temporary digestive adjustment or taste preferences rather than significant medical concerns.
- People with known allergies to Pistacia species or other tree resins
- Those with severe gallbladder disease or bile duct obstruction
- Individuals taking multiple medications without medical supervision
- Women who are pregnant or breastfeeding (due to limited safety data)
Pregnancy and Breastfeeding Concerns
While traditional use suggests mastic gum has been consumed by pregnant women in Mediterranean cultures for generations, formal safety studies specifically examining pregnancy and lactation are lacking. This research gap creates a cautionary situation where potential benefits must be weighed against theoretical risks. The prudent approach for pregnant and breastfeeding women involves avoiding therapeutic doses of mastic gum while awaiting more definitive safety data.
The concern stems not from documented adverse effects but rather from the principle of precaution regarding bioactive substances during these sensitive periods. Some compounds in mastic gum could theoretically affect hormonal balance or cross the placental barrier, though no specific mechanisms for harm have been identified. Women already using mastic gum who become pregnant should discuss continuation with healthcare providers, weighing individual health circumstances against theoretical concerns.
Medication Interactions to Watch For
Mastic gum contains compounds that may influence drug metabolism pathways, particularly those involving cytochrome P450 enzymes in the liver. This potential interaction warrants caution for individuals taking medications with narrow therapeutic windows, including certain anticoagulants, anticonvulsants, and immunosuppressants. Those taking multiple medications should consult healthcare providers before adding mastic gum to their regimen, particularly if their medication requires careful blood level monitoring.
Allergic Reactions: What to Look Out For
While rare, allergic reactions to mastic gum can occur, particularly in individuals with known sensitivities to other tree resins or members of the Anacardiaceae family (which includes pistachios, mangoes, and cashews). Typical allergic response signs include itching, rash, swelling (especially of lips, tongue, or throat), respiratory difficulty, or digestive distress occurring shortly after consumption. Anyone experiencing these symptoms should discontinue use immediately and seek appropriate medical attention, particularly if breathing is affected or symptoms are severe.
The Bottom Line: Is Mastic Gum Worth Trying?
When evaluating mastic gum’s potential place in your health regimen, the scientific evidence supports specific applications while suggesting caution for others. For digestive applications—particularly H. pylori management, functional dyspepsia, and general digestive comfort—substantial clinical evidence supports mastic gum’s effectiveness. Similarly, oral health applications stand on solid ground with multiple studies confirming benefits for plaque reduction and gingival health. These applications represent the “low-hanging fruit” where most users can reasonably expect positive outcomes.
For other applications like cholesterol management, anti-inflammatory support, and metabolic health, mastic gum offers promising but less definitive benefits. These areas show biological plausibility and preliminary evidence but may not provide dramatic results for all users. A reasonable approach involves viewing mastic gum as one component of a comprehensive health strategy rather than a standalone solution—particularly for complex chronic conditions. When sourced authentically and used appropriately, this ancient resin offers a valuable addition to modern wellness practices, bridging traditional wisdom and contemporary science in our pursuit of natural health solutions.
Frequently Asked Questions
As mastic gum continues gaining popularity in natural health circles, certain questions consistently emerge from those considering its use. Addressing these common concerns helps potential users make informed decisions and develop realistic expectations about this traditional remedy. The following questions represent those most frequently asked by consumers exploring mastic gum for various health applications.
Beyond addressing specific concerns, these questions help frame the broader context of mastic gum’s place in modern health practices. Understanding both capabilities and limitations allows for integration of this traditional remedy into contemporary wellness approaches without misconceptions or excessive claims that ultimately undermine credibility.
Can mastic gum completely cure stomach ulcers?
While mastic gum demonstrates significant anti-H. pylori activity, describing it as a “cure” for stomach ulcers oversimplifies a complex condition. Research shows mastic gum can reduce H. pylori bacterial load and improve ulcer symptoms, but complete bacterial eradication rates in studies typically range from 30-40%—lower than the 70-90% achieved with conventional triple antibiotic therapy. Additionally, not all ulcers stem from H. pylori infection, with some resulting from medication use, excessive stomach acid, or other factors that mastic may not directly address.
A more accurate perspective views mastic gum as a valuable complementary approach for ulcer management rather than a standalone cure. Many practitioners use it alongside conventional treatments to improve outcomes, reduce antibiotic requirements, or help prevent recurrence after standard treatment. For mild cases or preventative approaches, mastic alone may provide sufficient benefit, but severe or complicated ulcers typically require comprehensive medical management.
How long should I use mastic gum before expecting results?
Timeframes for observable benefits vary significantly based on the specific health application and individual factors. For digestive comfort issues like bloating, mild indigestion, or functional dyspepsia, many users report noticeable improvements within 7-14 days of consistent use. However, more significant goals like meaningful H. pylori reduction typically require at least 4-6 weeks of regular supplementation, with some studies suggesting optimal results after 8-12 weeks of daily use.
For systemic benefits like cholesterol management or anti-inflammatory effects, longer timeframes typically apply, with measurable changes often requiring 8-12 weeks of consistent supplementation. These gradual timelines reflect mastic gum’s gentle, regulatory effects on biological processes rather than the rapid, forced changes often seen with pharmaceutical interventions. Patience and consistency typically yield better long-term results than intermittent or short-term use.
Is authentic mastic gum only from Greece?
Yes, authentic medicinal-grade mastic gum specifically comes from the island of Chios in Greece, where the particular variety Pistacia lentiscus var. Chia grows in unique environmental conditions that maximize beneficial compound production. While related Pistacia species grow throughout the Mediterranean and Middle East, producing similar-appearing resins, the specific therapeutic profile documented in research derives from the Chios variety, which has earned Protected Designation of Origin (PDO) status from the European Union recognizing its unique properties.
Can children safely use mastic gum?
Traditional use suggests mastic gum has been given to children in Mediterranean cultures for generations, particularly for digestive complaints and dental health. However, formal safety studies specifically examining pediatric use are limited. For oral health applications, children old enough to safely chew gum without swallowing it (typically age 4+) can likely use small amounts of mastic gum under supervision, though commercial children’s toothpastes provide a more standardized approach to dental care.
For internal use addressing specific health concerns, consulting a pediatric healthcare provider represents the prudent approach, particularly for children under 12. If approved by healthcare providers, children typically require proportionally reduced dosages based on weight, often approximately 1/3 to 1/2 the adult dosage depending on age and size. As with adults, starting with minimal amounts and monitoring for any unusual responses allows for personalized assessment of tolerance.
Will mastic gum interfere with my prescription medications?
Mastic gum contains compounds that could potentially influence drug metabolism pathways, particularly those involving cytochrome P450 enzymes in the liver. This theoretical interaction warrants caution for individuals taking medications with narrow therapeutic windows, including certain anticoagulants, anticonvulsants, immunosuppressants, and some cardiac medications. Those taking such medications should consult their healthcare providers before adding mastic gum to their regimen.
For most common medications with wider therapeutic windows, significant interactions appear unlikely based on available evidence. However, the conservative approach involves informing all healthcare providers about mastic gum use, particularly when beginning or adjusting medication regimens. This transparency allows for appropriate monitoring and adjustment if needed, ensuring optimal outcomes from both conventional and natural approaches.
When properly sourced and used appropriately, mastic gum offers a valuable bridge between traditional wisdom and modern health practices. Its documented benefits for digestive and oral health make it a worthy consideration for those seeking natural approaches to these common concerns. While not a miracle cure, this ancient resin continues earning scientific validation for specific applications that align remarkably well with its centuries of traditional use.