Key Takeaways
- Gum disease progresses through four distinct stages – gingivitis, early periodontitis, moderate periodontitis, and advanced periodontitis – each with increasing severity and different treatment approaches.
- Early detection at the gingivitis stage is critical as it’s the only completely reversible stage, while later stages can lead to permanent damage including bone and tooth loss.
- Dentists use probing depth measurements (the space between gums and teeth) as a primary indicator of gum disease progression, with healthy measurements at 1-3mm and severe disease at 7+mm.
- ProHEALTH Dental specialists provide customized treatment plans for all stages of gum disease, from simple cleanings to advanced surgical interventions.
- Nearly half of American adults over 30 have some form of gum disease, with higher prevalence among men, smokers, and those below the poverty line.
Your gums are trying to tell you something. Those tender spots when brushing, the occasional bleeding, or that slight redness along your gumline aren’t just minor inconveniences – they’re early warning signs of a progressive condition that could threaten not just your smile, but your overall health.
Understanding the stages of gum disease empowers you to take action at the earliest signs, potentially saving your teeth and avoiding costly, complex treatments down the road. ProHEALTH Dental specializes in diagnosing and treating all stages of gum disease with personalized care approaches that address your specific needs.
The 4 Gum Disease Stages: What Your Mouth Is Trying to Tell You
Gum disease isn’t a sudden event but rather a continuum that worsens over time when left untreated. The progression follows a predictable pattern through four primary stages, each with distinct characteristics and increasing severity. Knowing these stages helps you recognize where you might be on this spectrum and understand the urgency of intervention.
While the technical term “periodontal disease” might sound intimidating, it simply refers to the infection and inflammation of the structures surrounding your teeth. As bacteria accumulate along and below your gumline, your body’s immune response triggers inflammation that, over time, can damage the supporting structures of your teeth. For more information on the stages of gum disease, you can refer to this insightful article.
The Centers for Disease Control and Prevention reports that nearly 47% of adults aged 30 and older have some form of periodontal disease, making it one of the most common chronic conditions in America. The prevalence increases with age, affecting over 70% of adults 65 and older.
Gum Disease By The Numbers:
– 47% of adults over 30 have some form of gum disease
– More common in men (56.4%) than women (38.4%)
– Higher prevalence in smokers (64.2%)
– More common in those below the poverty line (65.4%)
– Leading cause of adult tooth loss in the United States
Understanding Healthy Gums: Your Baseline for Comparison
Before diving into disease stages, it’s important to understand what healthy gums look like. Healthy gingival tissue appears firm, pink (though may have variations depending on ethnicity), and fits snugly around each tooth. When you brush or floss, healthy gums don’t bleed or feel tender. The gumline follows a consistent scalloped pattern around each tooth, creating what dentists call a “knife-edge” where the gum meets the tooth.
What Healthy Gums Look Like
Healthy gums are typically coral pink or salmon-colored in fair-skinned individuals, while those with darker complexions may have gums with natural melanin pigmentation appearing brown or even bluish. Regardless of base color, healthy gums should have a consistent hue, feel firm when touched, and have a stippled texture similar to an orange peel. The papillae (the triangular portion of gum between teeth) should be pointed and fill the space between teeth completely.
Perhaps most importantly, healthy gums maintain a tight seal around each tooth, with minimal space between the gum and tooth surface. This tight seal helps prevent bacteria from accessing the deeper structures that support your teeth.
The Critical Role of Gum Health in Overall Oral Health
Your gums serve as the foundation for your teeth, providing both protection and support. Like the foundation of a house, when this structure weakens, everything above it becomes unstable. Healthy gums anchor teeth firmly in place, protect the sensitive roots from decay and temperature sensitivity, and form a barrier against infection-causing bacteria that could otherwise enter your bloodstream.
How Dentists Measure Gum Health
During routine dental exams, your dentist or hygienist will use a specialized tool called a periodontal probe to measure the depth of the space between your gums and teeth. This measurement, taken at six points around each tooth, provides crucial information about your gum health. In healthy gums, these “pocket depths” typically measure between 1-3 millimeters. Measurements beyond this range often indicate gum disease progression. Additionally, your dental professional will note any bleeding during this probing, as bleeding is a key indicator of inflammation and early disease.
Stage 1: Gingivitis – The Warning Signs
Gingivitis marks the beginning of gum disease and is characterized by inflammation of the gums without yet affecting the underlying bone or connective tissue attachment. At this stage, the condition is completely reversible with proper care. Think of gingivitis as your mouth’s equivalent of a warning light on your car’s dashboard – it indicates a problem that needs attention before more serious damage occurs.
The primary cause of gingivitis is bacterial plaque – that sticky, colorless film that constantly forms on your teeth. When plaque isn’t removed through regular brushing and flossing, it irritates the gum tissue, triggering inflammation. Left unchecked, this plaque eventually hardens into tartar (calculus), which can only be removed by a dental professional.
Common Symptoms to Watch For
The telltale signs of gingivitis are often subtle but should never be ignored. Your gums may appear redder than usual, especially along the margins where they meet your teeth. You might notice swelling or puffiness, giving your gums a less firm appearance than healthy tissue. Perhaps the most common sign is bleeding during brushing or flossing – even slight bleeding isn’t normal and indicates inflammation.
Bad breath that persists despite brushing and using mouthwash can also signal gingivitis, as bacteria releasing odorous compounds multiply in the inflamed tissue. Some people report a metallic taste in their mouth or notice their gums feeling tender when brushing. At this stage, pocket depths typically remain within the healthy range of 1-3mm, but bleeding points during probing are present.
Stage 3: Moderate Periodontitis – Increasing Damage
When gum disease advances to moderate periodontitis, the infection begins to cause significant and potentially permanent damage. At this stage, the same symptoms as early periodontitis continue but with increased severity. The bacteria have now penetrated deeper beneath the gumline, attacking the supporting bone and ligaments that hold your teeth securely in place.
Without intervention at this stage, patients face a much higher risk of tooth loss as the foundation supporting the teeth weakens considerably. The infection creates a destructive cycle where bacteria trigger an immune response that inadvertently damages your own tissues in an attempt to fight the infection. For more information on the progression of gum issues, you can read about the 4 stages of gum disease.
Deeper Pockets (6-7mm) and What They Mean
Pocket depth measurements now reach 6-7 millimeters, creating significant spaces between teeth and gums where bacteria thrive in an oxygen-poor environment. These deeper pockets are particularly concerning because they’re nearly impossible to clean with regular brushing and flossing. The bacteria in these pockets produce toxins that accelerate tissue destruction and bone loss.
These deeper pockets also represent a critical turning point in disease progression because they increase the risk of bacteria entering your bloodstream. The pocket depth correlates directly with the severity of infection and inflammation, with each millimeter increase representing a substantial worsening of the condition.
Bone Loss and Tooth Mobility
X-rays at this stage typically reveal 30-50% bone loss around affected teeth. This bone destruction weakens the foundation that anchors your teeth, resulting in noticeable tooth mobility or shifting. You might notice spaces developing between teeth that weren’t there before, changes in your bite, or teeth that feel loose when you press on them with your tongue or finger.
Risk to Your Overall Health
The connection between moderate periodontitis and systemic health becomes increasingly concerning at this stage. Research has established links between periodontal disease and conditions like heart disease, diabetes, stroke, respiratory diseases, and pregnancy complications. The inflammation doesn’t stay contained in your mouth but can contribute to inflammatory processes throughout your body.
The bacteria from these deeper pockets have greater access to your bloodstream, potentially traveling to other sites in your body and triggering inflammatory responses elsewhere. For patients with diabetes, moderate periodontitis can make blood sugar control more difficult, creating a harmful cycle where each condition worsens the other.
More Aggressive Treatment Needs
Treatment at this stage requires more aggressive approaches, often including scaling and root planing (deep cleaning) with local anesthesia, followed by antimicrobial treatments to control bacterial growth. Your dentist may recommend more frequent professional cleanings, prescription-strength antimicrobial mouth rinses, and in some cases, localized antibiotic delivery directly into the periodontal pockets.
Stage 4: Advanced Periodontitis – Severe Consequences
Advanced periodontitis represents the final and most destructive stage of gum disease. At this point, the infection has caused extensive damage to the gums, periodontal ligaments, and supporting bone structure. The bacteria have created such significant destruction that teeth often become severely loose or even fall out.
Patients with advanced periodontitis often experience difficulty chewing, persistent bad breath that doesn’t respond to oral hygiene measures, and painful abscesses. The extensive inflammation can cause the gums to recede dramatically, making teeth appear longer than normal (“long in the tooth”) as the roots become exposed.
Deep Pockets Beyond 7mm
Pocket depths measuring beyond 7mm are hallmarks of advanced periodontitis. These extremely deep pockets harbor large populations of aggressive bacteria that continue destroying tissue. The depth of these pockets makes them completely inaccessible to home care methods and challenging even for professional cleaning.
At this stage, these deep pockets may develop into periodontal abscesses—painful, pus-filled infections that can cause severe pain, swelling, and fever. These abscesses represent acute infections that require immediate treatment and often serve as the event that finally brings patients in for care after years of progressive disease.
Significant Bone Loss and Tooth Loss Risk
X-rays typically show bone loss exceeding 50%, sometimes approaching 70-80% around severely affected teeth. This extensive bone destruction eliminates the structural support teeth need to remain stable, resulting in severe mobility, shifting, and ultimately tooth loss if left untreated.
Systemic Health Connections
The systemic health implications become even more pronounced at this advanced stage. The chronic inflammation and bacterial load place significant stress on your immune system and can exacerbate conditions like cardiovascular disease, diabetes, and rheumatoid arthritis. Some studies suggest links between advanced periodontal disease and increased risk of certain cancers, Alzheimer’s disease, and other serious health conditions.
Complex Surgical Interventions
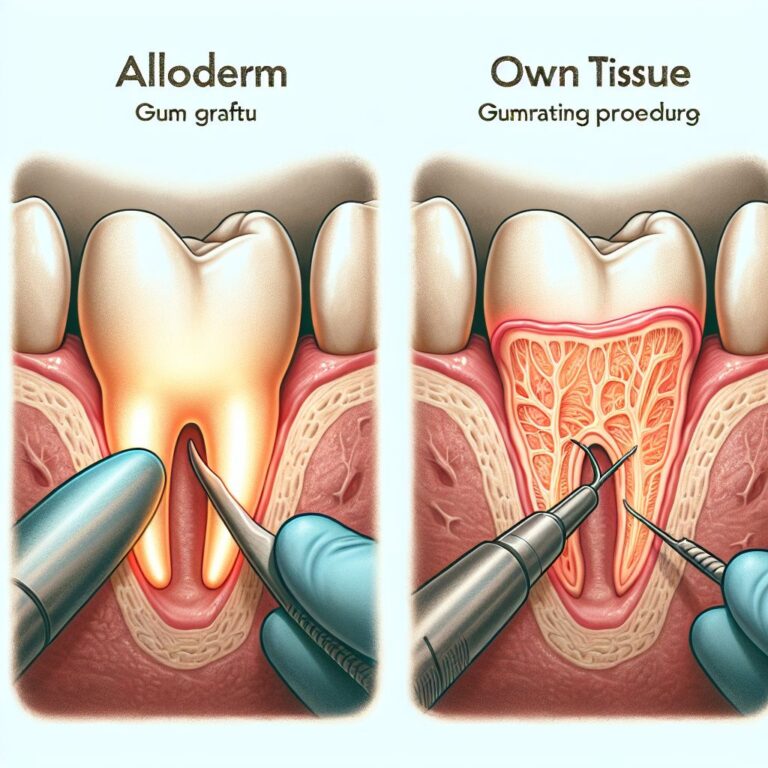
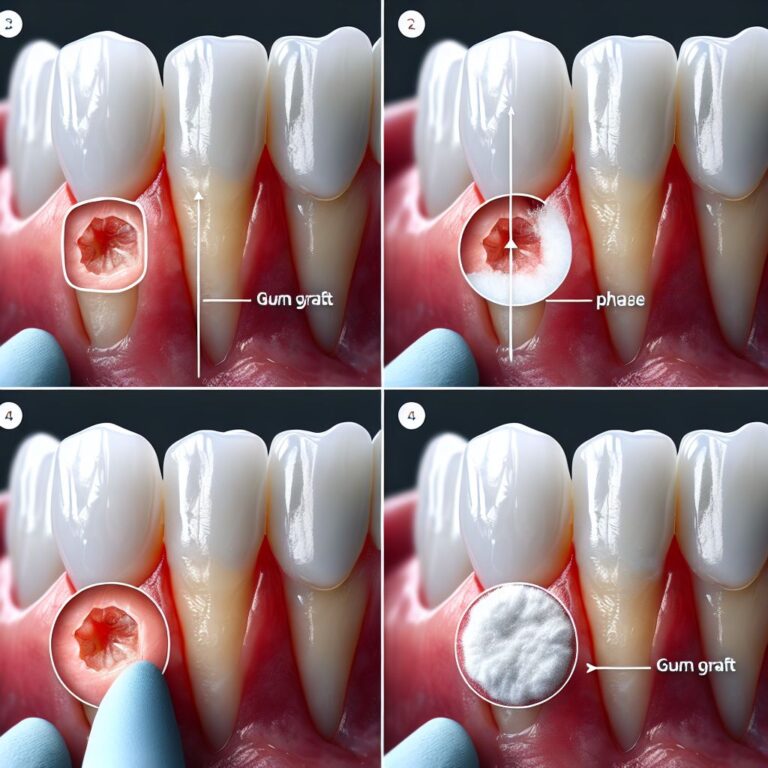
Treatment for advanced periodontitis typically requires specialized periodontal surgery, which may include flap surgery to access and clean deep pockets, bone grafting to rebuild lost bone, guided tissue regeneration to stimulate new bone growth, and in some cases, extraction of teeth that cannot be saved. Following surgical interventions, patients typically require ongoing maintenance therapy with frequent professional cleanings and evaluations to prevent disease recurrence.
How Dentists Chart Your Gum Health
Proper documentation of your periodontal condition is crucial for tracking disease progression or improvement over time. Dental professionals use a standardized charting system to record measurements around each tooth, creating a comprehensive map of your gum health.
This periodontal chart serves as your oral health baseline and helps guide treatment decisions. Modern dental offices often use digital charting systems that provide visual representations of your condition, making it easier to understand the state of your gum health and track changes between visits.
Understanding Probing Depths
The periodontal probe measures the depth of the space between your gum and tooth at six points around each tooth (three on the outer surface and three on the inner surface). These measurements are recorded in millimeters and provide critical information about attachment loss and disease severity. A healthy sulcus (the natural space between gum and tooth) typically measures 1-3mm, while measurements of 4mm or greater indicate disease progression.
Bleeding Points and What They Indicate
Your dental professional will note any spots that bleed during probing, as this is a key indicator of active inflammation. Bleeding on probing (BOP) suggests that the tissue is inflamed and the body is sending increased blood flow to the area as part of the immune response. The percentage of sites that bleed during examination helps determine the extent of active disease throughout your mouth.
Recession Measurements
Gum recession—the pulling away of gum tissue from the tooth—is another important measurement recorded during periodontal charting. Recession exposes the root surface of the tooth, which is more vulnerable to decay and can lead to sensitivity. This measurement helps track the progression of tissue loss over time.
Recession is measured from the cementoenamel junction (CEJ, the point where the enamel of the crown meets the cementum of the root) to the current gum margin. Increasing recession measurements indicate progressive tissue loss and often correlate with disease advancement.
The combination of probing depth and recession measurements gives what dentists call “clinical attachment loss”—the total amount of supporting structure that has been lost around a tooth. This composite measurement is one of the most important indicators of periodontal disease severity.
Using Digital and Color-Coded Charts
Many dental practices now use digital charting systems with color-coded displays that make it easier to visualize problem areas. Typically, these systems use green for healthy measurements (1-3mm), yellow for early disease (4-5mm), orange for moderate disease (6-7mm), and red for advanced disease (>7mm). This visual representation helps both dental professionals and patients understand the extent and location of periodontal problems at a glance.
Risk Factors That Speed Up Gum Disease
Certain factors can accelerate the progression of gum disease or make you more susceptible to developing it in the first place. Understanding these risk factors is crucial for prevention and personalized treatment planning. Tobacco use stands as perhaps the most significant modifiable risk factor, with smokers being up to six times more likely to develop periodontal disease than non-smokers. Other major factors include poorly controlled diabetes, which impairs healing and increases inflammation; genetic predisposition, which may make some individuals more susceptible despite good oral hygiene; hormonal changes during pregnancy or menopause; certain medications that reduce saliva flow or cause gum overgrowth; and chronic stress, which can weaken immune function.
Smoking and Tobacco Use
Tobacco use in any form—cigarettes, cigars, pipes, or smokeless tobacco—dramatically increases your risk of developing gum disease and accelerates its progression. The chemicals in tobacco products reduce blood flow to the gums, impairing their ability to heal and fight infection. Smokers typically show less obvious signs of inflammation (like bleeding), which can mask early disease and delay diagnosis until more advanced stages have developed. Research shows smokers are up to six times more likely to develop periodontitis than non-smokers and respond less favorably to treatment.
Diabetes and Blood Sugar Control
Diabetes and periodontal disease share a bidirectional relationship—each condition can worsen the other. Poorly controlled blood sugar weakens your immune system’s ability to fight infections, including those in your gums. High glucose levels in your saliva create an ideal environment for harmful bacteria to multiply. Additionally, diabetes causes blood vessel changes that reduce nutrient flow and waste removal from gum tissues, impairing healing and repair. Learn more about the stages of gum disease to better understand this connection.
Conversely, active periodontal disease makes blood sugar control more difficult, creating a harmful cycle of worsening symptoms in both conditions. Studies show that effective periodontal treatment can lead to improvements in glycemic control, highlighting the importance of coordinated care between your dentist and physician if you have diabetes. For more information on this, you can explore the stages of gum disease.
Genetics and Family History
Despite excellent oral hygiene, some individuals may be genetically predisposed to developing periodontal disease. Research suggests up to 30% of the population may have genetic factors that make them more susceptible to gum inflammation and breakdown. If your parents or siblings have a history of gum disease or early tooth loss, you may share genetic traits that increase your risk. These genetic variations often affect immune response, collagen production, or inflammatory processes.
Knowing your family history enables your dental team to implement more aggressive preventive strategies, including more frequent professional cleanings, earlier intervention at the first signs of disease, and possibly genetic testing to confirm susceptibility.
| Risk Factor | Impact on Gum Disease | Management Approach |
|---|---|---|
| Smoking | 6x higher risk, masks symptoms, reduces treatment success | Smoking cessation programs, more frequent cleanings |
| Diabetes | Bidirectional relationship, increased severity | Blood sugar control, coordination with physician |
| Genetics | Up to 30% of population has increased susceptibility | More aggressive prevention, possible genetic testing |
| Medications | Some cause dry mouth or gum overgrowth | Medication review, hydration strategies, specialized cleaning |
| Stress | Impairs immune function, promotes inflammation | Stress management techniques, more vigilant home care |
Understanding your personal risk profile allows for customized prevention strategies. Risk assessment isn’t about placing blame but rather identifying which factors require special attention in your oral health routine. Many dental offices now use risk assessment tools that consider multiple factors to develop personalized prevention and treatment plans.
For those with multiple risk factors, your dentist might recommend prescription-strength fluoride toothpaste, antimicrobial mouth rinses, or more frequent professional interventions to counterbalance these risks. Remember that even non-modifiable risk factors like genetics can be offset by more vigilant oral hygiene and professional care.
Medications That Affect Your Gums
Many common medications can adversely affect your gum health. Some medications, including certain antihypertensives, anticonvulsants, and immunosuppressants, can cause gingival hyperplasia—an overgrowth of gum tissue that creates deep pockets where bacteria thrive. Others, particularly antidepressants, antihistamines, and many pain medications, reduce saliva production, eliminating this natural protective mechanism against bacteria. Some medications also alter your microbiome or affect inflammatory responses. Always provide your dental team with a complete, up-to-date medication list so they can factor these influences into your treatment plan and recommend appropriate compensatory measures.
Stress and Immune Function
Chronic stress doesn’t just affect your mental wellbeing—it directly impacts your body’s ability to fight infection, including gum disease. Stress hormones like cortisol suppress immune function and promote inflammation throughout the body, including your gums. Additionally, people under stress often neglect oral hygiene routines, consume more inflammatory foods, or engage in harmful habits like teeth grinding that further damage periodontal structures. Incorporating stress management techniques like regular exercise, adequate sleep, mindfulness practices, or counseling can significantly improve not just your overall health but specifically your body’s ability to prevent and fight gum disease.
Your Action Plan for Healthy Gums at Any Stage
No matter where you currently are on the gum disease spectrum, taking action now can prevent further progression and, in many cases, reverse damage. The earlier you intervene, the better your outcomes will be. A comprehensive approach combines diligent home care, professional dental treatments, lifestyle modifications, and regular monitoring.
Remember that gum disease is largely preventable and manageable with the right approach. Even if you’ve already experienced some periodontal damage, implementing these strategies can help prevent further deterioration and maintain your remaining oral health. ProHEALTH Dental provides comprehensive periodontal care tailored to each stage of gum disease, from preventive measures to advanced surgical interventions.
Daily Oral Hygiene Must-Dos
Effective home care forms the foundation of gum disease prevention and management. Brush thoroughly twice daily for two minutes using a soft-bristled toothbrush and fluoride toothpaste, paying special attention to the gumline where bacteria accumulate. Position your brush at a 45-degree angle to your gums and use gentle circular motions rather than aggressive back-and-forth scrubbing that can damage gum tissue. Clean between your teeth daily using floss, interdental brushes, or water flossers—this step reaches the 40% of tooth surfaces that brushing alone misses.
For those with active gum disease, your dentist may recommend additional tools like rubber-tip stimulators to massage gum tissue, antimicrobial mouth rinses to reduce bacterial load, or specialized toothpastes formulated for gum health. Consistency matters more than perfection—maintaining these habits daily, even if imperfectly executed, provides significantly better outcomes than sporadic perfect cleaning.
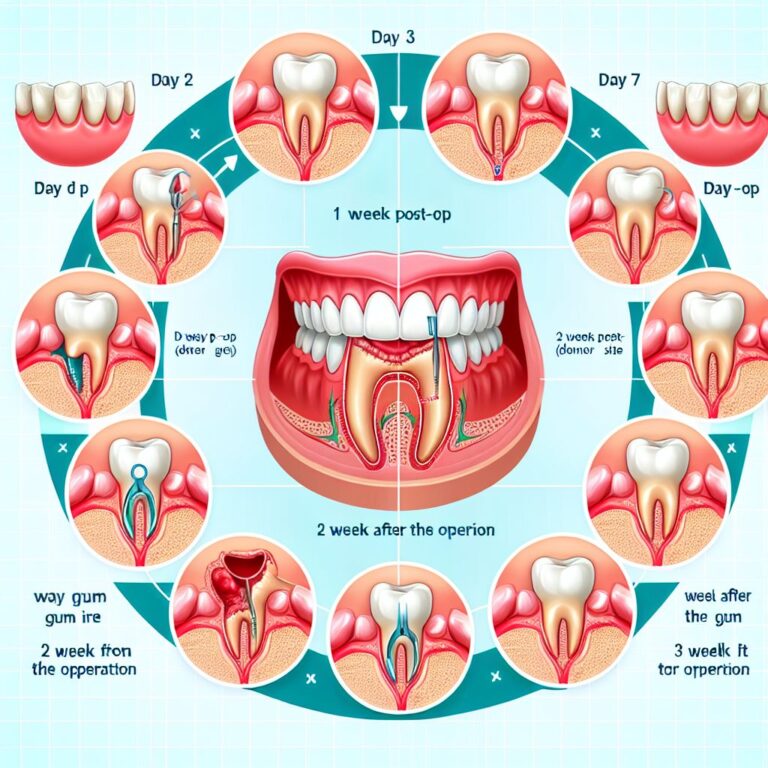
Professional Cleaning Schedule Based on Your Risk
While the standard recommendation for dental cleanings is twice yearly, patients with active gum disease or high-risk factors often require more frequent professional intervention. Your dentist might recommend a three or four-month cleaning schedule to disrupt bacterial colonies before they can cause significant damage. These more frequent interventions allow for regular reassessment of your condition and adjustment of your treatment plan as needed. For those with moderate to advanced periodontitis, your dentist might alternate between routine cleanings and more intensive deep cleanings (scaling and root planing) to maintain control of the disease.
Diet Changes That Support Gum Health
Your dietary choices significantly impact gum health beyond just avoiding sugary foods. Anti-inflammatory nutrients found in fruits, vegetables, fatty fish, nuts, and green tea help your body fight gum inflammation. Vitamin C is particularly important for gum tissue integrity and wound healing, while calcium and vitamin D support the bone structure that anchors your teeth. Conversely, a diet high in processed carbohydrates and sugars fuels bacterial growth and promotes inflammation. Staying well-hydrated also supports saliva production—your body’s natural defense against oral bacteria—while limiting alcohol consumption reduces dehydration and irritation of gum tissues. For more information on gum health, you can visit this insightful article on gum disease stages.
When to Seek Specialist Care
While general dentists can manage many cases of early to moderate gum disease, certain situations warrant referral to a periodontist—a specialist in gum health and disease. Consider specialist care if you have advanced disease with significant bone loss, recurring gum infections despite treatment, rapidly progressing disease, complicated medical conditions affecting gum health, or if you need advanced reconstructive procedures like bone grafting or guided tissue regeneration. Periodontists have additional years of specialized training beyond dental school focused exclusively on diagnosing and treating periodontal conditions and can offer advanced surgical techniques not typically performed in general practice.
Frequently Asked Questions
Understanding gum disease can be complex, and many patients have similar questions about prevention, progression, and treatment options. The following answers to common questions provide additional clarity on managing your periodontal health effectively.
Can gum disease be completely reversed?
Gingivitis, the earliest stage of gum disease, is completely reversible with proper professional cleaning and improved home care. Once the disease progresses to periodontitis (stages 2-4), the bone and attachment loss that occurs cannot be fully regenerated through non-surgical means alone. However, the disease process itself can be halted at any stage with appropriate intervention.
Even in advanced cases, surgical procedures like guided tissue regeneration and bone grafting can help regenerate some of the lost supporting structures, though typically not to their original, pre-disease levels. The goal of treatment in later stages focuses on stopping further progression, eliminating infection, and stabilizing the remaining support structures rather than complete reversal.
How quickly can I move from one stage to the next?
The progression rate from one stage to the next varies significantly between individuals based on risk factors, oral hygiene practices, and individual biology. For some individuals with high-risk factors like smoking or uncontrolled diabetes, progression from gingivitis to early periodontitis might occur within months. For others with good immune function and minimal risk factors, the disease might progress very slowly over many years or decades.
Progression isn’t always linear or constant—periods of active destruction may alternate with periods of stability. Factors like illness, increased stress, medication changes, or lapses in oral hygiene can trigger rapid acceleration of previously stable disease.
Regular dental evaluations are crucial for early detection of changes in your periodontal status. Your dentist can identify subtle shifts in measurements or inflammatory markers that indicate disease progression long before you notice symptoms, allowing for earlier intervention before significant damage occurs.
Are electronic toothbrushes better for preventing gum disease?
Research consistently shows that powered toothbrushes, particularly those with oscillating-rotating technology, remove more plaque and reduce gingivitis more effectively than manual brushing. The advantage is especially pronounced for people with limited dexterity, those wearing orthodontic appliances, or patients with periodontal disease. The built-in timers on most electric toothbrushes also encourage proper brushing duration, while pressure sensors help prevent the excessive force that can damage gum tissue. While a properly used manual toothbrush can be effective, electric toothbrushes generally make it easier to achieve optimal results with less perfect technique.
Does insurance cover periodontal treatment?
Most dental insurance plans provide some coverage for periodontal treatment, though the extent varies widely between policies. Typically, preventive care like regular cleanings receives the highest coverage (often 80-100%), while basic periodontal treatments like scaling and root planing might be covered at 50-80%. More advanced surgical procedures usually receive lower coverage, often around 50% if covered at all.
Many plans impose waiting periods for periodontal coverage, annual maximums that limit total benefits, and frequency limitations on certain procedures. Some medical insurance plans may provide coverage for periodontal treatment when it relates to management of certain systemic conditions like diabetes. The investment in treating gum disease early typically saves significant costs compared to delayed treatment that requires more extensive interventions or tooth replacement. ProHEALTH Dental’s administrative team can help you understand your coverage options and maximize your benefits.
Can children develop gum disease?
While chronic periodontitis primarily affects adults, children and adolescents can develop gingivitis and, rarely, more aggressive forms of periodontal disease. Puberty-associated gingivitis is common due to hormonal changes that increase gum sensitivity to plaque. Poor oral hygiene, mouth breathing, certain medications, and orthodontic appliances can increase a child’s risk of developing gum inflammation.
Some children may have genetic conditions or immune disorders that predispose them to more severe periodontal problems at an early age. Aggressive periodontitis, though rare, can affect adolescents and cause rapid bone loss around certain teeth, particularly the first molars and incisors.
Early detection through regular dental visits is especially important for children with risk factors. Teaching proper brushing and flossing techniques from an early age establishes lifelong habits that help prevent periodontal problems throughout life. If you notice signs of gum inflammation in your child—such as bleeding when brushing, gum redness, or bad breath—consult your pediatric dentist or family dentist promptly for evaluation and appropriate intervention.
For comprehensive care at any stage of gum disease, ProHEALTH Dental offers specialized treatment programs designed to restore your oral health and prevent disease progression. Our team stays at the forefront of periodontal treatment techniques to provide you with the most effective, comfortable care possible.
Understanding the stages of gum disease is crucial for maintaining oral health. Gum disease, also known as periodontal disease, progresses through several stages, each with its own set of symptoms and treatments. The initial stage, gingivitis, is characterized by inflammation of the gums and can often be reversed with proper dental care. As the disease progresses to periodontitis, the damage becomes more severe, leading to potential tooth loss if left untreated. For a detailed breakdown of the 4 stages of gum disease, it’s important to consult with dental professionals who can provide personalized care and advice.