Key Takeaways
- Healthy gums are the foundation of oral health, with daily proper brushing technique and consistent flossing being crucial first steps for improvement
- Adding antimicrobial mouthwash and staying hydrated can significantly accelerate gum healing and reduce inflammation
- Your diet directly impacts gum health – increasing vitamin C-rich foods while reducing sugary foods can show visible improvements within weeks
- Natural remedies like salt water rinses and oil pulling can complement traditional oral hygiene for enhanced results
- Recognizing warning signs that require professional attention can prevent minor gum issues from developing into serious periodontal disease
The Silent Crisis: Why Your Gums Need Immediate Attention
Your gums are quietly telling you something important. While you might focus on having white teeth and fresh breath, it’s the pink tissue supporting your teeth that truly determines your long-term oral health. Gum disease affects nearly 50% of adults over 30, yet many don’t realize they have it until significant damage has occurred. Left untreated, gingivitis (mild gum inflammation) progresses to periodontitis, which can lead to tooth loss and has been linked to serious health conditions including heart disease, diabetes, and respiratory problems.
The most alarming aspect of gum disease is its silent progression. Many people experience no pain until the advanced stages, when treatment becomes more difficult and expensive. The good news? Gum health can improve dramatically with consistent care, and positive changes can be visible in as little as two weeks. By implementing the right habits now, you can reverse early gum disease, prevent recurrence, and potentially avoid thousands in dental work.
What makes healthy gums so essential is their role as the protective barrier against bacteria entering your bloodstream. When gums become inflamed and bleed easily, they create pathways for oral bacteria to circulate throughout your body. This bacterial migration explains why poor gum health correlates with increased risk of systemic health issues. By prioritizing your gums today, you’re not just saving your smile – you’re investing in your overall wellbeing for years to come.
7 Daily Habits That Transform Gum Health in Just Weeks
The journey to healthier gums doesn’t require expensive treatments or complicated procedures. Simple daily habits, when consistently applied, create the foundation for remarkable improvement. These seven practices, when incorporated into your routine, can visibly transform your gum health in as little as 2-4 weeks. The key is consistency – these aren’t one-time fixes but lifestyle changes that protect your oral health for the long term.
1. Upgrade Your Brushing Technique
Most people brush incorrectly, unknowingly damaging their gums in the process. The optimal technique involves holding your toothbrush at a 45-degree angle to your gums and using gentle, circular motions rather than aggressive back-and-forth scrubbing. Spend at least two minutes brushing, dividing your mouth into four quadrants and dedicating 30 seconds to each. Focus especially on the gumline where bacteria tend to accumulate and cause inflammation. Remember that harder brushing doesn’t equal cleaner teeth – in fact, aggressive brushing is a leading cause of gum recession.
Timing matters too. While most people brush in the morning and before bed, the most critical brushing session is actually before sleep. During sleep, saliva production decreases, leaving your mouth more vulnerable to bacterial growth. Never skip your bedtime brush, and consider brushing about 30 minutes after meals rather than immediately after eating, especially if you’ve consumed acidic foods that temporarily soften enamel.
2. Make Flossing Non-Negotiable
No single habit impacts gum health more dramatically than daily flossing. Your toothbrush can only reach about 60% of your tooth surfaces, leaving the spaces between teeth as perfect hiding spots for bacteria and food particles. Traditional string floss remains the gold standard when used correctly – gently curve the floss around each tooth in a C-shape and slide it beneath the gumline without snapping it down (which can traumatize gum tissue). For those with dexterity issues or tight contacts between teeth, floss picks or water flossers provide excellent alternatives.
If you’ve avoided flossing because it causes bleeding, that’s actually a sign you need it most. Healthy gums don’t bleed when flossed. The bleeding indicates inflammation from bacterial buildup – and consistent flossing will typically resolve this issue within 1-2 weeks as gum health improves. A helpful tip for floss-avoiders: start by committing to floss just one tooth per night, then gradually increase until you’re flossing your entire mouth daily.
3. Add Antimicrobial Mouthwash to Your Routine
Strategic mouthwash use can significantly accelerate gum healing when added to your brushing and flossing routine. Look specifically for alcohol-free antimicrobial formulations containing ingredients like cetylpyridinium chloride (CPC) or essential oils like thymol. These target the bacteria responsible for gum inflammation without drying out oral tissues. For those with active gingivitis, a short-term chlorhexidine rinse (available by prescription) can dramatically reduce bacterial load and inflammation in just days.
Timing your mouthwash use properly maximizes its effectiveness. Rather than using it immediately after brushing (which can wash away the beneficial fluoride from your toothpaste), use mouthwash at a different time of day or wait at least 30 minutes after brushing. For optimal results, swish vigorously for a full 60 seconds, reaching all areas of your mouth, including the back molars where gum disease often begins. Some studies show that using mouthwash before brushing can loosen plaque, making your brushing more effective.
Mouthwash Type Comparison for Gum Health
Type Best For Key Ingredients Usage Duration Antimicrobial Daily prevention CPC, essential oils Long-term use Chlorhexidine Active gingivitis Chlorhexidine gluconate Short-term (2 weeks) Natural Mild inflammation Tea tree, aloe vera Long-term use Fluoride Cavity prevention Sodium fluoride Long-term use
4. Stay Hydrated for Natural Oral Cleansing
Water might be the most overlooked factor in gum health. Proper hydration ensures adequate saliva production, and saliva is your mouth’s built-in defense system. It contains antimicrobial compounds, helps neutralize acids, and physically washes away food particles and bacteria throughout the day. Aim for at least 8 glasses of water daily, with additional intake if you exercise or consume dehydrating beverages like coffee or alcohol. For more information on maintaining healthy gums, visit this comprehensive guide.
The benefits of staying hydrated extend beyond just increasing saliva flow. Drinking water after meals helps rinse away food particles when brushing isn’t possible. For enhanced gum health benefits, consider making water your primary beverage and significantly reducing sugary drinks. Even seemingly healthy options like fruit juices can feed the bacteria that contribute to gum inflammation. Remember that chronic dry mouth, whether from medication side effects or medical conditions, dramatically increases your risk of gum disease and requires proactive management.
5. Choose Gum-Friendly Foods
Your diet plays a crucial role in either fighting or feeding gum disease. Foods rich in vitamin C (citrus fruits, bell peppers, strawberries) are particularly beneficial as this vitamin is essential for collagen production and tissue repair in your gums. Studies show that vitamin C deficiency can lead to weakened gum tissue that’s more susceptible to bacterial infection. Similarly, foods high in antioxidants help combat inflammation throughout the body, including your gums.
Crunchy, fibrous foods like apples, carrots, and celery act as natural toothbrushes, physically scraping away plaque as you chew. They also stimulate saliva production, which helps neutralize acids and remineralize teeth. Meanwhile, fermented foods like yogurt, kefir, and kimchi introduce beneficial bacteria that can help maintain a balanced oral microbiome. On the flip side, minimize highly processed carbohydrates and sugary foods, which feed harmful bacteria and promote inflammation. When you do indulge, try to do so at mealtimes rather than snacking throughout the day, which subjects your gums to constant bacterial acid attacks.
- Gum-Healing Foods: Leafy greens, fatty fish (omega-3s), berries, green tea, fermented foods
- Foods That Harm Gums: Sugary snacks, soft drinks, refined carbohydrates, alcohol, sticky candies
- Surprise Gum Helpers: Shiitake mushrooms (contain lentinan, which fights plaque-causing bacteria), aged cheeses (help neutralize acid)
- Best Snacks for Gum Health: Nuts, raw vegetables, plain yogurt with berries, green tea
6. Quit Smoking and Limit Alcohol
Few things damage gum health more severely than smoking. Tobacco use reduces blood flow to the gums, masks symptoms of gum disease by suppressing bleeding, impairs healing, and creates an environment where harmful bacteria thrive. Studies consistently show that smokers are up to five times more likely to develop gum disease than non-smokers, and treatments are less effective when patients continue to smoke. The good news is that gum health begins improving within days of quitting, with former smokers eventually returning to a risk level similar to people who never smoked.
Excessive alcohol consumption similarly compromises gum health by dehydrating tissues, reducing saliva flow, and potentially leading to neglected oral hygiene. Additionally, many alcoholic beverages contain sugars that feed harmful bacteria. If you drink alcohol, do so in moderation (one drink daily for women, two for men), rinse with water between alcoholic drinks, and never skip your bedtime oral hygiene routine, regardless of how late you get home. For those serious about improving gum health, consider a 30-day break from alcohol to observe the difference in gum appearance and reduced morning breath.
7. Check for Grinding and Get a Nightguard if Needed
Teeth grinding (bruxism) places excessive force on your gums and supporting bone, accelerating gum recession and tooth mobility. Many people grind unconsciously during sleep, especially during periods of high stress. Signs include morning jaw pain, headaches, worn tooth surfaces, and notching near the gumline. If you suspect you might be grinding, consult your dentist about a custom nightguard – a protective appliance that creates a cushioning barrier between your upper and lower teeth.
While custom-fitted nightguards from your dentist provide the best protection, over-the-counter “boil-and-bite” options can offer temporary relief while you arrange a dental appointment. Additionally, stress-reduction techniques like meditation, regular exercise, and improved sleep hygiene can help reduce grinding frequency. For some patients, physical therapy or targeted jaw exercises can help relax the muscles involved in grinding. Addressing this often-overlooked factor can make a significant difference in your gum health improvement journey.
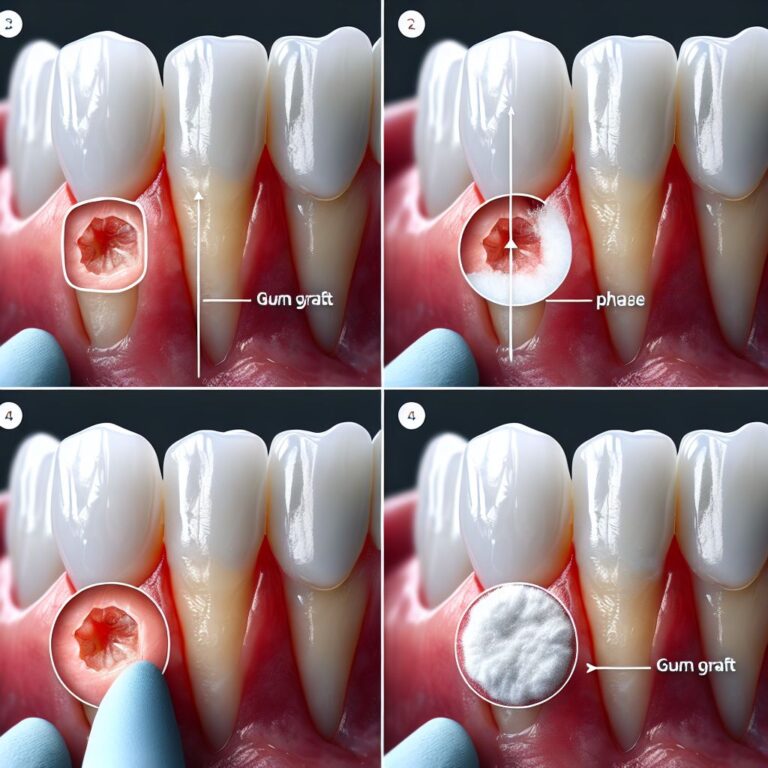
3 Professional Treatments That Speed Up Gum Recovery
While home care forms the foundation of gum health, professional interventions can dramatically accelerate healing, especially if you’re dealing with moderate to advanced gum issues. These treatments reach below the gumline where home care cannot, addressing the root causes of persistent inflammation. They’re particularly valuable for those who’ve struggled with gum disease despite good home care, or who want to jump-start their gum recovery process.
Professional treatments complement rather than replace your daily routine. They create a clean slate from which your enhanced home care can maintain optimal gum health. Most importantly, they provide access to specialized tools and medications that aren’t available for home use. Consider these interventions as strategic investments in your oral health that can potentially save thousands in more extensive treatments down the road.
1. Deep Cleaning (Scaling and Root Planing)
When gum disease progresses beyond what regular cleanings can address, scaling and root planing becomes necessary. This procedure goes beyond standard cleaning to remove hardened tartar deposits from below the gumline, where they create persistent inflammation. Using specialized instruments, dental professionals carefully clean the root surfaces, removing bacterial toxins and creating a smooth surface that discourages future bacterial attachment. The procedure is typically performed under local anesthesia for comfort, often one quadrant of the mouth at a time.
The results can be dramatic – studies show that scaling and root planing can reduce pocket depths (the space between tooth and gum) by 1-3mm in many cases. Bleeding on probing, a key indicator of inflammation, typically decreases by 50% or more within weeks. For optimal results, this treatment is often combined with antimicrobial rinses or placement of time-release antibiotics directly into deeper pockets. Most patients notice significantly firmer, pinker gums and reduced sensitivity within 2-3 weeks of treatment, though full healing continues for months.
2. Laser Therapy for Infected Gums
Dental laser therapy represents one of the most advanced treatments for gum disease, offering precision that traditional methods can’t match. These specialized lasers target infected tissue while preserving healthy gum tissue, significantly reducing bleeding, swelling, and discomfort compared to conventional treatments. The laser energy effectively eliminates bacteria while simultaneously stimulating the body’s natural healing processes, which can accelerate recovery by 30-50% compared to traditional methods.
The procedure itself is remarkably comfortable, often requiring minimal or no anesthesia. The laser creates a sterile environment as it works, reducing the risk of post-treatment infection and promoting faster attachment of gum tissue to tooth surfaces. Many patients report being able to return to normal activities immediately after treatment, with minimal dietary restrictions. While slightly more expensive than traditional therapies, the reduced discomfort and accelerated healing make laser treatment an increasingly popular option for those seeking faster results.
3. Professional-Grade Products on Prescription
Dentists can prescribe specialized products that deliver higher concentrations of therapeutic ingredients than over-the-counter options. Prescription-strength antimicrobial rinses containing chlorhexidine gluconate can reduce bacterial load by up to 90%, dramatically accelerating gum healing. For localized areas of persistent inflammation, antibiotic gels or microspheres placed directly into deep pockets can provide targeted therapy for up to 21 days, reaching areas that rinses cannot penetrate.
High-potency fluoride toothpastes containing sodium fluoride at 5000ppm (more than double the strength of over-the-counter options) not only strengthen enamel but also help reduce gingival inflammation in many patients. For those with severe sensitivity due to gum recession, prescription desensitizing pastes containing ingredients like potassium nitrate at therapeutic concentrations can provide relief while gums heal. These professional products are typically used for limited periods to jump-start recovery, after which maintenance can often be achieved with over-the-counter alternatives.
The Right Tools Make All the Difference
Your daily oral care tools significantly impact gum health outcomes. The right instruments can make your efforts more effective while minimizing damage to delicate gum tissue. Think of these tools as investments in your oral health that pay dividends through reduced inflammation, less bleeding, and ultimately, lower dental bills. For many people, upgrading even one aspect of their oral care toolkit leads to noticeable improvements within weeks.
Electric vs. Manual Toothbrushes: Which Helps Gums More?
Multiple clinical studies show that electric toothbrushes, particularly those with oscillating-rotating technology, remove up to 21% more plaque than manual brushing and reduce gingivitis by an average of 11% after just three months of use. The built-in timers ensure you brush for the full recommended two minutes, while pressure sensors prevent the excessive force that commonly causes gum recession with manual brushing. The consistent motion also removes plaque more effectively at the gumline, where it matters most for gum health.
If you prefer manual brushing or aren’t ready to invest in an electric model, select a soft-bristled brush with a small head that can reach all areas of your mouth. Replace any toothbrush that shows splayed bristles, as these indicate you’re applying too much pressure. Technique becomes even more critical with manual brushing – use gentle circular motions rather than aggressive scrubbing, and pay special attention to the junction where your teeth meet your gums. Regardless of which type you choose, replacement every three months ensures optimal cleaning power and prevents bacterial buildup on the brush itself.
Water Flossers: The Game-Changer for Reluctant Flossers
For those who find traditional flossing difficult or uncomfortable, water flossers offer a breakthrough alternative that’s clinically proven to be up to 50% more effective at reducing gingival bleeding than string floss. These devices direct a pulsating stream of water between teeth and below the gumline, dislodging bacteria and food particles without the manual dexterity required for traditional flossing. They’re particularly valuable for people with orthodontic appliances, dental implants, or bridges where string floss can’t easily reach.
When selecting a water flosser, look for models with adjustable pressure settings (starting low if you have sensitive gums) and ADA approval. For maximum benefit, use lukewarm water or add a capful of alcohol-free antimicrobial mouthwash to the reservoir. Direct the stream at a 90-degree angle to the tooth surface, pausing briefly between teeth and giving special attention to areas that tend to bleed or collect food. While water flossers excel at removing loose debris, they work best as a complement to, rather than a complete replacement for, traditional flossing techniques.
Gum Massage Tools That Stimulate Healing
Specialized gum massage tools stimulate blood circulation to gum tissue, accelerating the delivery of nutrients and immune cells needed for healing. Options range from simple rubber-tipped stimulators to more advanced devices that combine massage with cleaning functions. Regular gum massage has been shown to increase tissue keratinization (toughening the outer layer), making gums more resistant to bacterial invasion and mechanical damage. For more insights on maintaining healthy gums, check out ways to keep gums healthy.
For a basic approach, rubber-tipped stimulators can be used after brushing, applying gentle circular pressure along the gumline. More advanced options include silicone brushes that fit over your fingertip for precise control. Even the simple practice of gentle gum massage with a clean finger after brushing can improve circulation and resilience. These tools are particularly beneficial for areas showing early signs of recession or those recovering from active inflammation.
Best Toothpastes for Gum Repair
Not all toothpastes are created equal when it comes to gum health. Look for formulations containing stannous fluoride, which offers antimicrobial properties in addition to cavity prevention. Studies show that stannous fluoride toothpastes can reduce gingival bleeding by up to 57% compared to regular sodium fluoride formulations. Other beneficial ingredients include zinc citrate, which helps control plaque buildup, and potassium nitrate for those experiencing sensitivity due to gum recession.
Avoid toothpastes containing sodium lauryl sulfate if you have recurring canker sores or sensitive gum tissue, as this foaming agent can irritate delicate oral mucosa. Similarly, approaches with excessive whitening compounds can increase sensitivity in exposed root surfaces. For severely inflamed gums, toothpastes containing natural anti-inflammatories like aloe vera or chamomile can provide soothing relief while your gums heal. Regardless of which formulation you choose, ensure it carries the ADA Seal of Acceptance, which confirms both safety and effectiveness.
Natural Remedies That Actually Work for Gum Health
While professional care and daily hygiene form the foundation of gum health, certain natural approaches have demonstrated genuine benefits in clinical studies. These remedies can complement conventional care, particularly for those seeking additional support between dental visits or preferring natural alternatives where possible. The most effective natural approaches target the underlying causes of gum inflammation: bacterial overgrowth and the body’s inflammatory response.
Salt Water Rinses: The Simple Solution That Works
This time-tested remedy reduces inflammation through osmosis, drawing out fluid from swollen tissues while creating an environment less hospitable to harmful bacteria. Mix half a teaspoon of sea salt in 8 ounces of warm water and rinse vigorously for 30 seconds, two to three times daily. The saline concentration creates a temporary change in fluid balance that helps reduce swelling, while the warm temperature increases circulation to accelerate healing.
Salt water rinses are particularly effective after flossing or when experiencing mild gum irritation. They’re completely safe for daily use and can be especially beneficial during the early stages of implementing your improved oral hygiene routine, when gums may be more sensitive and reactive. For enhanced effects, consider adding a drop of tea tree oil or a teaspoon of raw honey (used after rinsing, not swallowed) for additional antimicrobial properties.
Oil Pulling: Ancient Technique with Modern Benefits
This Ayurvedic practice involves swishing oil (typically coconut or sesame) in your mouth for 15-20 minutes to reduce harmful bacteria. Research shows that oil pulling can significantly reduce plaque and gingivitis scores when practiced consistently. The mechanical action of swishing helps dislodge bacteria, while fatty acids in the oils may disrupt bacterial cell membranes. Additionally, coconut oil contains lauric acid, which has demonstrated antimicrobial properties against some oral pathogens.
For best results, use one tablespoon of organic, cold-pressed oil first thing in the morning before eating or drinking. Swish gently rather than vigorously to avoid tiring your jaw muscles, and never swallow the oil, which contains toxins and bacteria pulled from your mouth. While not a replacement for brushing and flossing, oil pulling can serve as an effective supplementary practice, particularly for those experiencing chronic mild inflammation despite good oral hygiene.
Tea Tree Oil Applications
Tea tree oil contains powerful compounds that combat the bacteria responsible for gum disease. Studies show that toothpastes containing tea tree oil significantly reduce gingival bleeding and inflammation compared to conventional formulations. The oil’s natural antimicrobial properties target the specific bacteria that trigger gum disease while its anti-inflammatory components help soothe irritated tissue.
To use safely, add 1-2 drops to your regular toothpaste or mix a single drop with a tablespoon of carrier oil (such as coconut oil) for a gentler application. Commercial mouthwashes containing properly diluted tea tree oil are also available. Never use undiluted tea tree oil directly on gum tissue, as it can cause irritation, and avoid swallowing products containing this potent essential oil. For those with sensitive tissues, a patch test is recommended before regular use.
Aloe Vera for Gum Inflammation
The same aloe vera renowned for soothing skin irritations offers remarkable benefits for inflamed gums. Research demonstrates that aloe gel applied topically reduces gingival inflammation and accelerates healing through its combination of anti-inflammatory compounds, antioxidants, and vitamins. It’s particularly effective for healing after deep cleaning procedures and for managing chronic gum irritation.
For gum application, use only 100% pure, food-grade aloe vera gel without added preservatives or flavors. Apply a small amount directly to affected gum areas using a clean finger or cotton swab after brushing, allowing it to sit for several minutes before rinsing gently. Some holistic dentists also recommend drinking a small amount of aloe vera juice daily for its internal anti-inflammatory benefits, though this should be discussed with your healthcare provider, particularly if you take medications that might interact with aloe’s compounds.
Vitamin C and Other Supplements That Strengthen Gums
Vitamin C plays a critical role in gum health by promoting collagen production, strengthening blood vessels, and enhancing immune function. Clinical studies show that people with low vitamin C levels have significantly higher rates of periodontal disease. While food sources like citrus fruits, bell peppers, and strawberries provide excellent natural vitamin C, supplementation of 500-1000mg daily can accelerate gum healing, particularly for those with deficiencies or active inflammation.
Beyond vitamin C, coenzyme Q10 has shown promise for gum health, with research indicating it can reduce pocket depth and bleeding in patients with periodontal disease. Omega-3 fatty acids from fish oil or algae sources help modulate the inflammatory response throughout the body, including gum tissue. Zinc supports tissue healing and immune function, while vitamin D plays a crucial role in maintaining the integrity of the bone supporting your teeth. For comprehensive support, consider a supplement regimen that includes these key nutrients, ideally under the guidance of a healthcare provider familiar with nutritional approaches to oral health.
Red Flags: When to See a Dentist Immediately
While many mild gum issues respond well to improved home care, certain symptoms require professional evaluation without delay. These warning signs indicate potentially serious conditions that can progress rapidly, leading to permanent damage if not addressed promptly. Remember that pain is not always present even with significant gum disease, so visual changes and bleeding patterns are often more reliable indicators of problems requiring intervention.
Persistent Bleeding Even After Improved Care
If your gums continue to bleed despite two weeks of diligent brushing, flossing, and antimicrobial rinses, professional evaluation is necessary. While initial bleeding when starting improved care is normal, persistent bleeding suggests deeper infection or inflammation that home care alone cannot resolve. This is particularly concerning if the bleeding occurs spontaneously (without provocation from brushing or flossing) or seems to be increasing rather than decreasing over time. For more information on maintaining gum health, you can read about ways to keep gums healthy.
Bleeding that appears localized to specific areas rather than generalized throughout your mouth may indicate focused infection or even abnormal tissue growth requiring biopsy. In rare cases, persistent gum bleeding can also signal systemic health issues affecting blood clotting, including certain medications, vitamin deficiencies, or blood disorders. A dental professional can determine whether your symptoms warrant deeper periodontal treatment or medical referral.
Receding Gumline or Exposed Tooth Roots
Gum recession – where the margin of gum tissue surrounding teeth wears away or pulls back – exposes more of the tooth root and creates pockets where bacteria can accumulate. Unlike other gum conditions, recession typically doesn’t improve with home care alone once it has occurred. If you notice teeth appearing longer, increased sensitivity to hot or cold, or visible notching where the gum meets the tooth, seek professional evaluation promptly.
Early intervention for recession is crucial because, unlike gingivitis, natural regrowth of receded gum tissue is limited. Dental professionals can provide treatments ranging from desensitizing agents for exposed roots to surgical gum grafting procedures that restore the protective gum coverage. They can also identify and address the underlying causes of your recession, which might include overly aggressive brushing, genetic factors, misaligned teeth, or advanced periodontal disease.
Severe Pain or Abscess Formation
Intense gum pain, swelling with pus formation, or a pimple-like bump on the gums indicates a potential abscess – a pocket of infection that requires immediate treatment. These infections can spread rapidly to surrounding tissues and, in severe cases, enter the bloodstream, creating serious systemic health risks. Other warning signs include fever, facial swelling, or a foul taste/odor that persists despite brushing and rinsing.
- Emergency Symptoms: Facial swelling, difficulty swallowing or breathing, fever above 101°F accompanying gum pain
- Urgent Symptoms: Pus discharge, severe throbbing pain, obvious abscess or bubble on the gum
- Concerning Symptoms: Sudden tooth mobility, rapid onset of severe sensitivity, metallic taste
- Temporary Relief Measures: Salt water rinses, OTC pain relievers, cold compress (while seeking care)
Never attempt to “pop” or drain an abscess yourself, as this can spread infection. Avoid placing aspirin directly on the gum tissue, which can cause chemical burns. Instead, take appropriate pain medication orally while arranging for the earliest possible dental appointment. Most dental offices reserve space for emergency patients and will accommodate truly urgent situations within 24 hours.
Remember that dental infections rarely resolve without professional intervention, and delayed treatment often results in more extensive and expensive procedures. What begins as a simple infection requiring antibiotics can progress to requiring root canal therapy or even extraction if left untreated. When severe symptoms appear, timely professional care is both the most conservative and most economical approach.
For those without a regular dentist or dental insurance, community health centers and dental schools often provide emergency services at reduced costs. Many private dentists also offer payment plans for urgent care. The investment in addressing these warning signs promptly almost always saves money compared to the cost of treating advanced conditions.
Your 14-Day Gum Healing Plan
This structured two-week program creates progressive improvement in gum health through gradually introducing evidence-based practices. The plan builds new habits systematically, making sustainable change more likely than attempting to implement everything at once. Many patients notice significant reductions in bleeding and inflammation by day 7, with continued improvement through day 14 and beyond. For best results, continue these practices after the initial 14-day period as your new standard oral care routine.
The plan works by first controlling the most immediate sources of inflammation, then gradually introducing more advanced techniques to accelerate healing and prevent recurrence. Throughout the process, pay close attention to how your gums respond – decreasing sensitivity, reduced redness, and diminished bleeding all indicate positive progress. Take photos of your gums at days 1, 7, and 14 to visually track the improvements, which can provide powerful motivation to maintain your new habits.
Frequently Asked Questions
The journey to improved gum health naturally raises questions about expectations, techniques, and long-term outcomes. These evidence-based answers address the most common concerns patients express when beginning a gum health improvement program. Understanding these aspects of gum recovery can help you maintain realistic expectations while still achieving significant improvements in your oral health.
Remember that individual responses vary based on your starting condition, consistency with the recommended practices, and biological factors like immune function and genetic predisposition. What remains consistent across all patients, however, is that proactive gum care yields substantial benefits for oral health, comfort, and long-term tooth preservation.
How quickly can I expect to see improvements in my gum health?
Most people notice the first signs of improvement within 5-7 days of implementing consistent oral hygiene practices. The earliest changes typically include reduced bleeding during brushing and flossing, followed by decreased redness and swelling. By the two-week mark, gums often appear pinker, firmer, and contour more tightly around teeth. These visible changes reflect the resolution of superficial inflammation as bacterial loads decrease in response to improved care.
More significant healing, particularly for moderate to advanced gum disease, follows a longer timeline. Deeper pocket reduction typically requires 2-3 months of consistent care, while bone regeneration in areas of previous loss may take 6-12 months or longer. Patience and consistency are crucial, as gum healing follows a biological timeline that cannot be rushed. Regular dental check-ups during this period provide objective measurements of your progress and help identify any areas requiring additional attention.
Can damaged gums grow back or heal completely?
Gum tissue has limited regenerative capacity compared to some other body tissues. In cases of gingivitis (early-stage gum disease), complete healing is possible since the damage is confined to the soft tissue without affecting the underlying bone. When you improve oral hygiene and eliminate the bacteria causing inflammation, gum tissue can return to its healthy state within weeks, with normal color, texture, and contour.
For periodontitis (advanced gum disease) where bone loss has occurred, natural regrowth is limited. The gum tissue may heal and tighten around teeth, reducing pocket depths, but it typically won’t regrow to cover previously exposed root surfaces without surgical intervention. Specialized procedures like guided tissue regeneration and bone grafting can stimulate partial regeneration in carefully selected cases. The key takeaway is that prevention and early intervention yield the best outcomes, as advanced damage may not be fully reversible even with optimal care.
Receding gums specifically have minimal natural regenerative capacity. Once gum tissue has receded, exposing root surfaces, it generally won’t grow back on its own. Professional treatments like gum grafting can restore coverage to exposed roots, but these are surgical procedures requiring specialist care. This limited regenerative capacity makes prevention of recession through proper brushing technique and regular professional care especially important.
Healing Timeline for Different Gum Conditions
Condition First Improvements Significant Recovery Maximum Improvement Mild Gingivitis 3-7 days 2-3 weeks Complete healing possible Moderate Periodontitis 7-14 days 2-3 months Significant improvement, but some changes permanent Severe Periodontitis 14-21 days 3-6 months Stabilization and partial recovery, permanent changes remain Gum Recession Reduced inflammation: 7-14 days No natural regrowth Requires surgical intervention for coverage
Are electric toothbrushes really better for gum health than manual ones?
Clinical research consistently demonstrates superior plaque removal and gum health outcomes with electric toothbrushes compared to manual brushing. A landmark Cochrane Review analyzing 56 studies found that electric toothbrushes reduced plaque by 21% and gingivitis by 11% after three months compared to manual brushing. The benefits were even more pronounced for oscillating-rotating models. These advantages stem from consistent bristle movement, built-in timers ensuring adequate brushing duration, and pressure sensors that prevent the excessive force commonly applied with manual brushes.
That said, technique remains crucial regardless of brush type. A properly used manual toothbrush can maintain excellent gum health, while an improperly used electric toothbrush may cause damage. The key advantage of electric models is that they simplify proper technique, making optimal results more accessible for the average person. For those with dexterity issues, arthritis, or a history of aggressive brushing, the benefits of switching to an electric toothbrush are particularly significant. If cost is a concern, prioritize proper technique with a soft-bristled manual brush until an electric model becomes affordable.
Electric vs. Manual Toothbrush Comparison
Feature Electric Advantage Manual Advantage Plaque Removal Superior (especially at gumline) Adequate with proper technique Ease of Use Requires minimal technique Requires mastering proper method Cost Higher initial investment More economical Pressure Control Built-in sensors prevent damage Requires self-monitoring Special Needs Better for limited dexterity Portable, no charging needed
For those transitioning to an electric toothbrush, allow 1-2 weeks for your gums to adjust to the new cleaning action. Initial minor bleeding is normal as gums adapt to more thorough cleaning. Use the lowest intensity setting initially, gradually increasing as comfort permits. Remember that even with an electric toothbrush, the recommended brushing time remains two minutes, divided equally among all quadrants of your mouth.
The most significant benefits come from consistent daily use rather than the specific model chosen. A basic electric toothbrush used properly twice daily will yield better results than an expensive model used sporadically or incorrectly. When selecting an electric toothbrush, prioritize comfort, ease of use, and features that encourage consistent habits over marketing claims about specialized technologies.
How does diet specifically impact gum health?
Your diet affects gum health through multiple mechanisms, creating either an environment that promotes healing or one that accelerates inflammation and bacterial growth. Sugar and refined carbohydrates feed the bacteria that form plaque, producing acids that irritate gum tissue and demineralize tooth structure. Meanwhile, nutrient-dense foods provide the building blocks for tissue repair and immune function. Studies show that diets high in omega-3 fatty acids, antioxidants, and vitamin C correspond with significantly lower rates of periodontal disease, while diets high in processed carbohydrates correlate with increased inflammation and more rapid disease progression.
Is it normal for gums to bleed slightly when I first start flossing?
Yes, initial bleeding when beginning to floss regularly is completely normal and actually indicates you need to floss more, not less. Healthy gums don’t bleed when flossed, so the bleeding signals the presence of inflammation from bacterial buildup in areas your toothbrush can’t reach. This reaction typically subsides within 7-14 days of consistent daily flossing as inflammation resolves and gum tissue becomes healthier and more resilient.
If bleeding persists beyond two weeks of daily flossing, review your technique – you may be using too much pressure or snapping the floss against your gums rather than gently sliding it. Try using waxed floss, which moves more smoothly between teeth, or consider a water flosser as an alternative. Persistent bleeding limited to specific areas might indicate deeper issues requiring professional attention, particularly if accompanied by tenderness, swelling, or visible changes in the gum tissue.
DentaTech’s comprehensive gum health solutions have helped thousands improve their periodontal health using clinically-proven approaches. For personalized guidance on addressing your specific gum health concerns, visit our website for expert resources and product recommendations designed to support your journey to healthier gums.