Key Takeaways: Successful Gum Grafting for Dental Implants
- Healthy gum tissue around dental implants prevents bone loss and implant failure by creating a protective biological seal
- The ideal candidate for gum grafting shows exposed implant threads, thin tissue biotype, or aesthetic concerns in the smile zone
- Colorado Gum Care specializes in three main types of grafts for implants: connective tissue grafts, free gingival grafts, and acellular dermal matrix
- Recovery typically spans 1-2 weeks with complete healing occurring within 4-6 weeks with proper care
- Successful grafting significantly improves long-term implant success rates and aesthetic outcomes
Dental implants represent the gold standard for tooth replacement, but their long-term success depends heavily on the health and stability of surrounding gum tissue. When insufficient gum tissue exists around an implant, a gum graft becomes necessary to ensure proper healing, function, and aesthetics. At Colorado Gum Care, we’ve perfected the art and science of gum grafting over implants to provide our patients with optimal outcomes.
Gum recession around implants presents unique challenges compared to natural teeth. Unlike natural teeth that connect to surrounding tissues through periodontal ligaments, dental implants integrate directly with bone and rely on healthy gum tissue to create a protective seal. Without adequate gum tissue, implants become vulnerable to bacterial invasion, inflammation, and eventual failure – making proper graft procedures essential for long-term success.
“Successful implant therapy isn’t just about osseointegration – the soft tissue interface is equally critical. A well-executed gum graft creates the biological seal necessary for implant longevity and aesthetic satisfaction.” – American Academy of Periodontology
Why Your Implant Needs Healthy Gum Tissue
Dental implants differ fundamentally from natural teeth in how they interact with surrounding tissues. While natural teeth connect to the jawbone through periodontal ligaments, implants fuse directly with bone through osseointegration. This distinction makes the surrounding gum tissue even more critical for implant health and longevity.
Healthy gum tissue creates what periodontists call a “biological seal” around the implant. This seal serves as the first line of defense against bacteria that could otherwise travel down the implant surface and cause peri-implantitis – the implant equivalent of gum disease. When gum tissue is inadequate, thin, or receding, this protective barrier becomes compromised, putting your investment at risk. To learn more about maintaining healthy gums, you can explore gum grafting procedures and how they can help.
Beyond the functional benefits, sufficient gum tissue around implants also provides crucial aesthetic advantages. Thin or receding gums can reveal the metallic components of the implant, creating a “gray line” at the gumline that detracts from an otherwise natural-looking tooth replacement. In the smile zone especially, adequate pink gum tissue framing white tooth restorations creates the harmonious appearance patients desire.
The 5 Best Practices for Gum Grafts Over Implants
At Colorado Gum Care, we’ve developed a systematic approach to gum grafting for implants based on decades of clinical experience and the latest scientific evidence. Our five best practices ensure predictable results with minimal patient discomfort and maximum long-term benefits.
1. Comprehensive Pre-Surgical Assessment
Before recommending any graft procedure, we conduct a thorough evaluation of your implant site and overall oral health. This assessment includes detailed measurements of existing gum tissue thickness, width of keratinized tissue, position of nearby anatomical structures, and evaluation of your tissue biotype. We utilize advanced imaging technologies including cone-beam CT scans and digital impressions to create a precise surgical plan tailored to your specific needs.
During this assessment phase, we also evaluate whether the graft should be performed before implant placement (pre-implant), simultaneously with implant surgery, or after the implant has integrated (post-implant). This timing decision significantly impacts treatment outcomes and is determined based on your unique clinical situation rather than a one-size-fits-all approach.
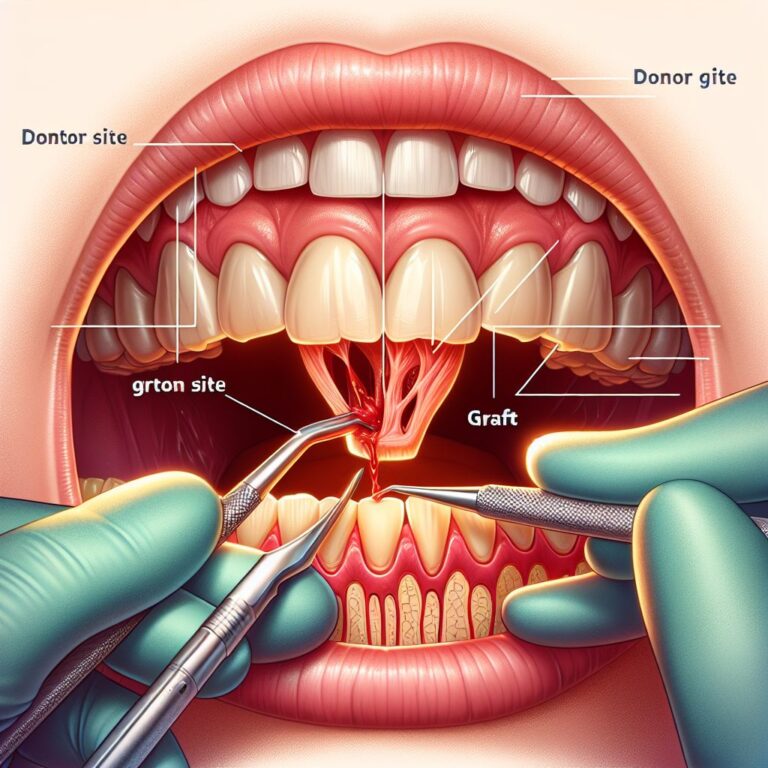
2. Selecting the Right Graft Material
The success of any gum graft over an implant largely depends on choosing the appropriate graft material. We carefully select between autogenous tissue (from your own palate), allograft (donor tissue), or xenograft (animal-derived) based on multiple factors including the location of your implant, the amount of tissue needed, and your personal preferences. Our experience shows that autogenous connective tissue typically yields the most predictable results, but modern alternatives now offer excellent outcomes with reduced surgical morbidity.
When harvesting tissue from your palate isn’t ideal, we utilize premium biocompatible alternatives that stimulate your body’s natural healing processes. These advanced materials have revolutionized gum grafting by eliminating the need for a second surgical site while still achieving excellent tissue volume and quality around implants.
3. Precision Surgical Techniques
Our microsurgical approach to gum grafting minimizes trauma and maximizes precision. Using specialized instruments and magnification, we meticulously prepare the recipient site around your implant to ensure optimal blood supply to the grafted tissue. This attention to detail creates an ideal environment for tissue integration and healing, significantly improving graft success rates.
For implants in aesthetically critical areas, we often employ the “tunnel technique” – a minimally invasive approach that allows us to place the graft material through small incisions without exposing the entire surgical area. This technique preserves existing blood vessels, reduces scarring, and accelerates healing while achieving superior aesthetic results.
4. Advanced Suturing Methods
Secure and precise suturing is essential for graft stability during the critical early healing phase. We employ microscopic suturing techniques with materials as fine as human hair to secure grafted tissue without creating tension or restricting blood flow. Our specialized suturing methods also help position the graft material for optimal thickness and contour around your implant, creating natural-looking results once healing is complete.
Beyond traditional interrupted sutures, we utilize advanced techniques like horizontal mattress, sling, and continuous locking sutures to stabilize different types of grafts in their ideal positions. This customized approach to wound closure significantly improves graft predictability while minimizing post-operative discomfort and accelerating healing times.
5. Structured Post-Operative Care
Your recovery experience and ultimate graft success depend heavily on proper post-operative care. We provide comprehensive instructions along with prescription medications to manage discomfort and prevent infection. Our structured follow-up protocol includes scheduled checkups at key healing milestones to monitor your progress and address any concerns promptly.
To optimize healing, we often incorporate advanced wound healing modifiers like platelet-rich fibrin (PRF) derived from a small sample of your own blood. This natural concentrate of growth factors accelerates tissue regeneration and improves the quality of healed gum tissue around your implant. We may also recommend specific supplements, antimicrobial rinses, and dietary modifications tailored to support optimal tissue healing throughout your recovery period.
When Is Gum Grafting Necessary for Your Implant?
Not every dental implant requires gum grafting, but certain clinical situations almost always benefit from this procedure. Understanding these indicators helps patients appreciate why we recommend grafting in specific cases to protect their implant investment long-term.
Exposed Implant Threads
When the threaded metal surface of an implant becomes visible, immediate intervention is necessary. Exposed implant threads not only create aesthetic concerns but also provide a direct pathway for bacteria to enter the implant-bone interface. This bacterial invasion can quickly lead to inflammation, bone loss, and eventual implant failure if not addressed promptly. Our gum grafting procedures provide complete coverage of exposed implant components, restoring both function and appearance while preventing further complications.
Thin Tissue Biotype
Patients with naturally thin gum tissue face higher risks for implant complications. This genetic tissue characteristic provides insufficient protection against mechanical stress and bacterial challenges, often leading to recession, inflammation, and aesthetic concerns around implants. We assess tissue thickness using specialized measurement tools during your consultation.
When we identify a thin tissue biotype, preventive grafting significantly reduces complication risks by creating a thicker, more resilient gum tissue barrier around your implant. This proactive approach prevents future recession and creates a more stable environment for long-term implant success, particularly in patients with aggressive oral hygiene habits or teeth grinding tendencies.
Aesthetic Concerns in the Smile Zone
Implants in the visible front teeth area demand meticulous attention to gum tissue aesthetics. Even minor recession or tissue deficiencies can create noticeable asymmetry, color differences, or unnatural contours that compromise your smile. Gum grafting in the aesthetic zone focuses on creating natural-looking papillae (the triangular gum tissue between teeth), proper gum height, and harmonious tissue thickness that frames your implant restoration beautifully.
For patients seeking truly exceptional aesthetic outcomes, we often combine gum grafting with custom provisional restorations that gradually shape the surrounding tissue into ideal contours. This comprehensive approach to implant aesthetics ensures that both the white (tooth) and pink (gum) components of your smile appear completely natural and harmonious.
Types of Gum Grafts We Use for Implants
The success of implant therapy often depends on selecting the most appropriate graft technique for each unique clinical situation. At Colorado Gum Care, we specialize in three primary graft types, each with specific advantages for different implant scenarios.
Connective Tissue Grafts
Connective tissue grafts represent our most frequently used technique for implant cases requiring significant tissue augmentation. This approach involves harvesting a section of connective tissue from beneath the palatal surface, creating a dual-layer that promotes exceptional thickness and stability. The subepithelial harvesting technique minimizes donor site discomfort while providing superior tissue quality around the implant.
This graft type excels in cases requiring both increased tissue thickness and width, making it our preferred choice for implants in the aesthetic zone. The rich blood supply and cellular composition of connective tissue grafts lead to predictable integration and natural-looking results that maintain stability over time.
Free Gingival Grafts
For implant cases lacking adequate keratinized tissue – the firm, attached gum tissue necessary for implant health – free gingival grafts offer an effective solution. This technique utilizes a full-thickness piece of palatal tissue that includes both epithelium and connective tissue to create a band of tough, resilient gingiva around the implant. While slightly more uncomfortable during healing than other options, free gingival grafts provide unmatched durability in areas exposed to mechanical stress or where minimal keratinized tissue exists.
We typically reserve this technique for posterior implants or cases where tissue thickness is adequate but width of attached gingiva is deficient. The distinctive appearance of free gingival grafts makes them less suitable for highly visible areas but ideal for functional enhancement around implants experiencing tissue mobility issues.
Acellular Dermal Matrix
For patients seeking to avoid palatal tissue harvesting, acellular dermal matrix provides an excellent alternative. These processed donor materials maintain the structural framework necessary for your cells to populate and revascularize the graft site. We utilize premium acellular products that undergo rigorous processing to ensure safety while preserving the essential matrix properties that support tissue regeneration.
This approach offers significant advantages including unlimited material availability, consistent thickness, and elimination of donor site discomfort. Our experience shows particularly good results when using these materials for implant site development prior to implant placement and for covering minor thread exposure in non-aesthetic areas.
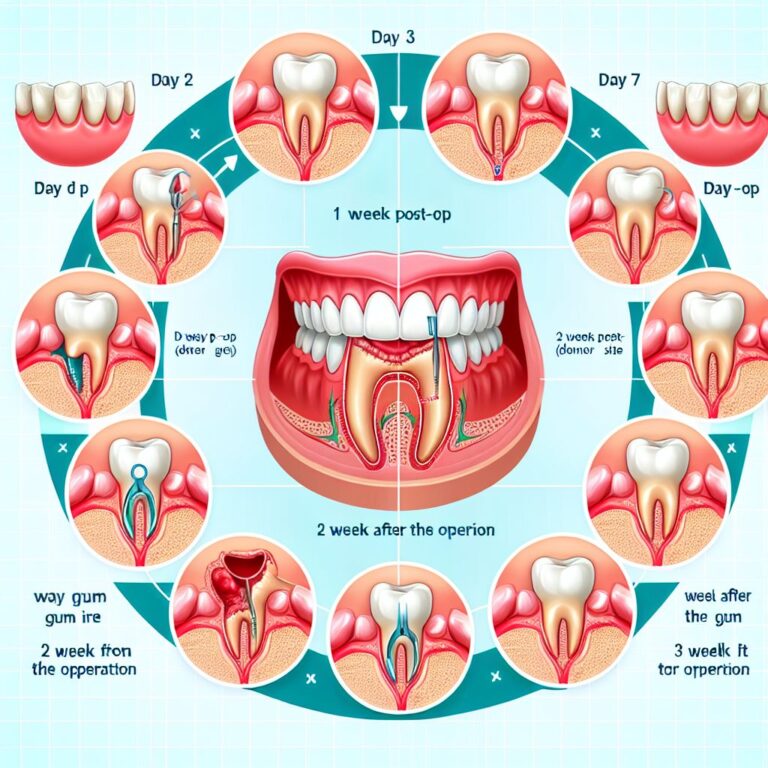
Your Recovery Timeline After Implant Gum Grafting
Understanding what to expect during recovery helps our patients navigate the healing process with confidence. While individual experiences vary, most gum grafts over implants follow a predictable healing timeline with proper care.
First 48 Hours
The initial post-operative period focuses on clot formation and protection of the newly placed graft. Expect minor bleeding that diminishes within 24 hours and moderate discomfort managed effectively with prescribed medications. We recommend cold compresses applied in 20-minute intervals to reduce swelling, along with a soft, cool diet that avoids the surgical area.
During this critical period, avoid any activity that could disrupt the graft, including rinsing vigorously, smoking, or touching the area. The specialized dressing we place over most grafts provides protection and should remain undisturbed until your follow-up appointment, typically scheduled 24-48 hours after surgery to verify proper initial healing.
Weeks 1-2
By the end of the first week, initial graft attachment is well underway as new blood vessels begin forming within the grafted tissue. Most sutures remain in place during this period to ensure graft stability while initial integration occurs. Discomfort typically subsides significantly by day 5-7, allowing most patients to resume normal activities with careful precautions around the surgical site.
During your week-one checkup, we’ll assess healing progress and may remove certain sutures if appropriate. We’ll also provide guidance on transitioning to a more normal diet and modified oral hygiene routine that protects the developing graft while maintaining cleanliness. Most patients can resume work and social activities during this phase, though we recommend continued caution with strenuous exercise until after the two-week mark.
Complete Healing Phase
Full maturation of a gum graft around an implant typically requires 4-6 weeks, though the tissue continues to remodel for several months. By the 3-4 week point, the graft should appear well-integrated with surrounding tissues, though some redness may persist. Most patients can resume normal oral hygiene practices and dietary choices by this stage, though we recommend continued gentle care of the grafted area.
Your final follow-up appointment around the 6-week mark allows us to evaluate the completed healing process and verify the success of the procedure. At this point, we can assess whether the graft has achieved the desired tissue thickness, width of keratinized tissue, and aesthetic integration with surrounding tissues – the three primary metrics we use to determine graft success around implants.
Real Results: How Gum Grafts Improve Implant Success
The benefits of properly executed gum grafts extend far beyond immediate aesthetic improvements. Long-term studies demonstrate significantly higher implant survival rates when adequate soft tissue surrounds the implant. Our internal data shows that implants with grafted soft tissue demonstrate a 94% success rate at 10-year follow-up compared to 83% for non-grafted sites with thin tissue biotypes.
Beyond longevity, patients report greater satisfaction with grafted implants due to improved appearance, reduced sensitivity, and easier maintenance. The investment in proper soft tissue management pays dividends through fewer complications, less bone loss, and more natural-looking results that maintain their quality over decades rather than years.
Frequently Asked Questions
Throughout our years of specializing in implant-related soft tissue procedures, we’ve encountered numerous questions from patients considering gum grafts for their implants. Below, we address the most common concerns to help you make informed decisions about your treatment options.
These answers reflect our clinical experience with thousands of graft procedures, though your individual situation may require personalized recommendations during consultation. We encourage patients to bring their questions and concerns to their appointments so we can provide specific guidance for their unique needs.
Is gum grafting painful when done over an implant?
Most patients experience only mild to moderate discomfort following gum grafting over implants. The procedure itself is performed under profound local anesthesia, ensuring you feel no pain during treatment. Post-operative discomfort typically peaks at 24-48 hours before gradually subsiding over the next few days. We provide appropriate pain management medications and detailed instructions to minimize discomfort during recovery. Many patients report that the procedure was much more comfortable than they anticipated, particularly when donor tissue alternatives are used instead of palatal harvesting.
How long should I wait after implant placement to get a gum graft?
The optimal timing for gum grafting around implants depends on several clinical factors including the reason for grafting and the implant location. In many cases, we perform soft tissue grafting simultaneously with implant placement to minimize overall treatment time and surgical interventions. However, certain situations may require either pre-implant grafting or delayed grafting after osseointegration is complete.
- Pre-implant grafting: Recommended when the available soft tissue is severely deficient and would compromise implant positioning
- Simultaneous grafting: Ideal for most cases with moderate tissue deficiencies to prevent recession during healing
- Delayed grafting (3-6 months post-implant): Preferred when addressing recession that developed after implant placement or when focusing on final aesthetic refinements
During your consultation, we’ll evaluate your specific situation and recommend the most appropriate timing for your graft procedure. Our treatment recommendations prioritize long-term success while minimizing the number of surgical interventions needed.
Many factors influence this decision, including the initial stability of your implant, bone quality at the site, whether the implant is immediately loaded with a temporary crown, and your overall healing capacity. We carefully weigh these factors when creating your personalized treatment plan.
Can my body reject the gum graft material?
True rejection of gum graft material is extremely rare, particularly with autogenous grafts (using your own tissue). When using donor materials like acellular dermal matrix, these products undergo extensive processing to remove all cellular components while preserving the collagen framework, essentially eliminating rejection risk. What patients sometimes mistake for “rejection” is actually poor graft take due to inadequate blood supply, infection, or mechanical disruption during healing. Our meticulous surgical protocols, including proper site preparation, tension-free closure, and protective measures during healing, ensure the highest possible success rates for all graft materials used.
Will my dental insurance cover gum grafting for my implant?
Insurance coverage for implant-related gum grafting varies significantly between providers and plans. Many dental insurance policies provide partial coverage for soft tissue grafts when documented as medically necessary to preserve implant health, typically covering 50-80% of the procedure up to your annual maximum. However, grafts performed primarily for aesthetic enhancement often receive limited or no coverage. Our insurance specialists will verify your benefits before treatment and provide a detailed breakdown of expected coverage and out-of-pocket costs.
For patients with limited insurance benefits, we offer several financing options to make treatment accessible. Our team works diligently to maximize your insurance benefits while providing transparent information about treatment costs. We believe that financial concerns should never prevent patients from receiving necessary care to protect their implant investment.
How do I know if my implant needs a gum graft?
Several clinical signs may indicate the need for gum grafting around your existing implant. The most obvious is visible implant threads or a gray discoloration showing through thin gum tissue. Other indicators include progressive recession around the implant, inflammation that persists despite good oral hygiene, food impaction around the implant, or aesthetic concerns with the implant appearance. During your examination, we’ll measure the width of keratinized tissue and tissue thickness around your implant to determine if these fall below the thresholds associated with long-term implant health.
Early intervention typically yields the best results, so we recommend evaluation at the first sign of tissue changes around your implant. If you’re noticing that your implant looks longer than it used to, experiences more sensitivity, or doesn’t match your natural teeth aesthetically, these may be signs that gum grafting could be beneficial.
At Colorado Gum Care, we specialize in preserving and enhancing the soft tissue around dental implants through advanced grafting techniques. Our comprehensive approach ensures that your implant not only integrates successfully with the bone but also maintains healthy, attractive gum tissue for long-term function and aesthetics. To learn if gum grafting could benefit your dental implant, contact our office today for a personalized consultation with our implant soft tissue specialists.