Key Takeaways
- Light therapy for gum health uses specific wavelengths (405nm blue light and 810nm near-infrared) to target harmful bacteria and reduce inflammation in periodontal pockets.
- Dual-light antibacterial photodynamic therapy (aPDT) shows promising results in clinical studies, especially when combined with traditional mechanical cleaning.
- The Lumoral device is one of the leading gum health light therapy systems that combines photosensitizing mouth rinse with targeted light application.
- Light therapy is not a replacement for professional dental care but may serve as an effective complementary treatment for periodontal disease.
- While initial research is encouraging, more long-term studies are needed to fully validate the effectiveness of light therapy for various gum conditions.
Struggling with bleeding gums, periodontal disease, or receding gum lines? You’ve likely encountered advertisements for light therapy devices promising revolutionary results for your oral health. But before investing hundreds of dollars in these high-tech gadgets, it’s crucial to separate fact from marketing fiction.
The field of light therapy for gum health has grown significantly in recent years, with devices like the Lumoral leading the charge in bringing clinical photodynamic technology into home care routines. These devices claim to eliminate harmful bacteria, reduce inflammation, and promote healing in ways traditional brushing and flossing cannot achieve alone.
The Truth About Light Therapy for Gum Health
Light therapy for gum health isn’t new in dental offices, but the technology has only recently become available for home use. The treatment uses specific light wavelengths to target bacterial infections and inflammation in the gums. Unlike some wellness trends with little scientific backing, photodynamic therapy for periodontal health has a growing body of research supporting its effectiveness.
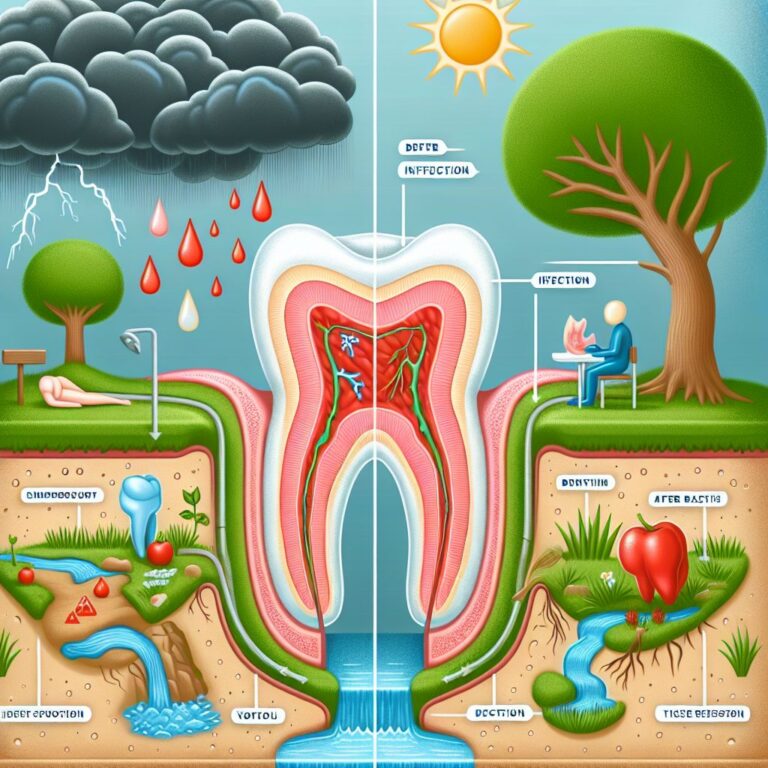
The most significant advantage of gum light therapy is its ability to reach areas traditional cleaning methods can’t access effectively. Periodontal pockets—spaces between teeth and gums that deepen with gum disease—harbor bacteria that cause ongoing inflammation. Light therapy can penetrate these spaces, potentially reducing bacterial load where brushing and flossing fall short.
However, it’s important to note that light therapy devices are intended to complement, not replace, conventional dental care. Regular dental check-ups, professional cleanings, and daily mechanical cleaning remain the foundation of good oral health.
How Gum Light Therapy Actually Works
Gum light therapy operates on the principle that certain wavelengths of light can affect biological tissues in beneficial ways. The technology leverages two main approaches: direct light application and photodynamic therapy, which combines light with photosensitizing agents.
Red Light Technology (630-660nm Wavelengths)
Red light therapy uses low-level wavelengths in the 630-660nm range, which penetrate tissue to potentially stimulate cellular repair and reduce inflammation. When applied to gum tissue, these wavelengths may help accelerate healing and strengthen the periodontal attachment. The light is believed to enhance mitochondrial function in cells, boosting energy production that supports tissue regeneration.
Most devices marketed for home use incorporate red light, often claiming it can improve circulation in the gums. While some clinical evidence supports these claims, the results vary significantly between individuals. Red light typically doesn’t directly kill bacteria but instead focuses on supporting the body’s natural healing processes.
Photodynamic Therapy with Mouth Rinses
The more advanced approach combines light with photosensitizing mouth rinses containing compounds like indocyanine green. These compounds attach to bacterial cell membranes and become activated when exposed to specific light wavelengths. Upon activation, they produce reactive oxygen species that effectively destroy bacterial cell walls.
This targeted antibacterial approach, known as antibacterial Photodynamic Therapy (aPDT), offers a significant advantage: it can eliminate harmful bacteria without promoting antibiotic resistance. Clinical studies have shown that aPDT can reduce bacterial load in periodontal pockets by up to 99% when properly applied.
The effectiveness depends largely on proper application technique and ensuring the photosensitizing agent reaches the infected areas before light activation. Most professional-grade systems require careful timing between rinse application and light exposure.
The Dual-Light Approach
The most advanced systems, like the Lumoral Clinic device, employ dual-light technology that combines 405nm blue light and 810nm near-infrared light. The blue light primarily works on surface bacteria, while the near-infrared wavelength penetrates deeper into periodontal tissues. This comprehensive approach allows treatment of both supragingival plaque (above the gum line) and subgingival bacteria in periodontal pockets.
The Lumoral device utilizes 48 high-power LEDs in a mouthpiece design to deliver this dual-wavelength treatment. What makes this approach particularly effective is the transgingival light application method, which allows light to penetrate through the periodontal tissue into the periodontal pocket. While the 405nm blue light has limited tissue penetration, the 810nm near-infrared component can reach deeper infections.
Case Study Highlight: A 78-year-old male patient with severe periodontal disease (Stage IV, Grade B) showed remarkable improvement after incorporating dual-light aPDT treatment into his daily oral hygiene routine. The treatment involved mechanical cleaning twice daily complemented by the dual-light therapy. After consistent use, periodontal pockets showed significant reduction and bleeding was substantially decreased.
Scientific Evidence Behind Light Therapy Devices
The efficacy of light therapy for gum health isn’t just marketing hype—there’s legitimate scientific research backing these treatments. Clinical studies have demonstrated that when properly applied, photodynamic therapy can significantly reduce bacterial loads in periodontal pockets and improve overall gum health markers. Most research focuses on the combination of photosensitizing agents with specific light wavelengths rather than light therapy alone.
Clinical Study Results on Bleeding Gums
Bleeding on probing (BOP) is one of the most reliable indicators of active gum inflammation. Multiple studies have shown that patients using photodynamic therapy experience significant reductions in bleeding sites compared to control groups. In one randomized clinical trial, participants receiving photodynamic therapy alongside scaling and root planing showed a 29% greater reduction in bleeding sites than those receiving mechanical cleaning alone.
The results are particularly impressive for patients with moderate to severe periodontitis who don’t respond adequately to conventional treatments. The anti-inflammatory properties of the near-infrared light appear to work synergistically with the antibacterial effects of the photosensitizing agents, creating a comprehensive approach to gum disease management.
Research on Periodontitis Treatment
Periodontitis represents a more advanced stage of gum disease involving bone loss and potential tooth mobility. A double-blind, randomized, split-mouth clinical trial published in dental journals demonstrated that laser and LED procedures adjunctive to scaling and root planing produced statistically significant improvements in periodontal pocket depth. Patients receiving the combined therapy showed a mean pocket depth reduction of 2.1mm compared to 0.9mm in the control group after six months.
Perhaps most encouraging is a four-year follow-up study that demonstrated the durability of these results when light therapy was incorporated into regular maintenance protocols. Patients maintained healthier gum attachment levels and experienced fewer periodontal disease recurrences than those receiving only standard care.
Limitations of Current Studies
Despite promising results, current research has several limitations worth noting. Many studies have relatively small sample sizes, and longer-term investigations spanning multiple years are still limited. Additionally, there’s significant variation in treatment protocols, devices used, and wavelength combinations across studies, making direct comparisons challenging.
Another important limitation is that most research has been conducted in clinical settings under professional supervision rather than with home-use devices. The effectiveness of self-administered light therapy may differ substantially from professionally applied treatments. Finally, most studies have focused on light therapy as an adjunct to conventional care rather than as a standalone treatment, suggesting its role is complementary rather than primary.
Popular Light Therapy Devices on the Market
Lumoral Device (Dual-Light aPDT)
The Lumoral device stands out as one of the most extensively researched oral light therapy systems available to consumers. This Finnish innovation uses a dual-light approach combining 405nm blue light with 810nm near-infrared light delivered through a mouthpiece containing 48 high-power LEDs. What makes Lumoral unique is its comprehensive photodynamic therapy system that includes a photosensitizing mouth rinse (Lumorinse) containing indocyanine green as the active compound.
The treatment protocol involves rinsing with the photosensitizing solution, which adheres to bacterial biofilms, followed by a 10-minute light application session. Clinical data suggests the system can reduce harmful bacteria by targeting them with reactive oxygen species generated when light activates the photosensitizing agent. Users typically report noticing reduced bleeding and improved gum appearance after 1-2 weeks of consistent daily use, though results vary based on individual conditions.
LED-Based Oral Devices
Beyond the Lumoral, several other LED-based oral devices have entered the market, though many lack the dual-wavelength approach or photosensitizing agents. These devices typically rely solely on red light therapy (630-660nm) and make more modest claims about improving circulation and reducing inflammation. Most feature mouthpiece designs that deliver light to the entire oral cavity simultaneously, though the intensity and coverage uniformity vary significantly between models.
Price Range and Accessibility
Gum health light therapy devices represent a significant investment, with prices ranging from $200 for basic LED mouthpieces to over $1,000 for comprehensive systems like the Lumoral that include photosensitizing agents. This high cost barrier means they’re primarily accessible to those with disposable income or severe gum conditions not responding to conventional treatments. Most devices are not covered by dental insurance plans, though some manufacturers offer payment plans or satisfaction guarantees to mitigate the financial risk for consumers.
Potential Risks and Side Effects
While light therapy for gum health is generally considered safe when used as directed, it’s not entirely without risks. Most adverse effects are mild and temporary, typically occurring when devices are misused or when patients have underlying conditions that make them particularly sensitive to light therapy. Understanding these potential risks is essential for making an informed decision about incorporating these devices into your oral care routine.
Burns and Tissue Damage
Thermal burns represent the most common adverse effect associated with improper use of light therapy devices. Most commercial units are designed with safety limits on heat generation, but extended contact with a single area or using devices with damaged components can potentially cause tissue irritation. Symptoms of thermal damage include persistent redness, swelling, or sensitivity that doesn’t resolve within 24 hours after treatment.
The risk increases with higher-intensity devices, particularly those using concentrated beams rather than diffused light. Following manufacturer guidelines regarding treatment duration is crucial, as exceeding recommended exposure times significantly increases burn risk. Patients with thin gum tissue or existing oral lesions should use these devices with particular caution and potentially consult their dental professional before beginning treatment.
Eye Safety Concerns
Important Safety Warning: Never look directly at LED or laser light sources in oral devices. Even brief exposure to high-intensity therapeutic light can potentially damage retinal cells. Always keep eyes closed when using intraoral light devices and follow all manufacturer safety instructions regarding eye protection.
Light therapy devices emit intense illumination that could potentially harm the retina if directed into the eyes. Though most devices are designed to minimize light leakage outside the mouth, improper handling could result in accidental eye exposure. Manufacturers typically recommend keeping eyes closed during treatment sessions as an additional precaution.
Some professional-grade systems include protective eyewear, but many consumer devices don’t provide this accessory. The risk varies by wavelength—blue light (405nm) poses greater potential for retinal damage than red or near-infrared wavelengths. If you experience any visual disturbances after using a light therapy device, discontinue use and consult an eye care professional immediately.
Children require particular supervision when using these devices due to their tendency to play with and potentially misuse technology. Most manufacturers specify minimum age requirements, typically recommending against use by children under 12 years old without direct adult supervision.
For those with photosensitivity disorders or taking medications that increase light sensitivity, additional caution is warranted, and medical clearance should be obtained before beginning treatment.
Who Should Avoid Light Therapy
Several patient groups should exercise caution or avoid oral light therapy altogether. Pregnant women are typically advised against using these devices due to insufficient safety data rather than known risks. Individuals with active oral cancers or precancerous lesions should absolutely avoid light therapy, as certain wavelengths might potentially stimulate abnormal cell growth. Additionally, patients with photosensitivity disorders like lupus or those taking medications like tetracycline antibiotics, certain antipsychotics, or St. John’s Wort should consult healthcare providers before using light therapy devices.
Individuals with dental implants should also consult their dentist before beginning light therapy. While no direct contraindication exists, the interaction between specific wavelengths and implant materials hasn’t been extensively studied. Those with pacemakers or other electronic medical implants should verify device compatibility, though most oral light therapy units produce minimal electromagnetic interference at levels unlikely to affect medical devices.
Real Benefits vs. Marketing Claims
With the growing popularity of oral light therapy devices, distinguishing between evidence-backed benefits and exaggerated marketing claims has become increasingly important. While legitimate benefits exist, manufacturers sometimes stretch the truth about what these devices can actually accomplish.
The most credible research supports using light therapy as an adjunctive treatment rather than a replacement for conventional dental care. Understanding these nuances helps set realistic expectations about what these devices can and cannot do for your gum health.
What Light Therapy Can Actually Improve
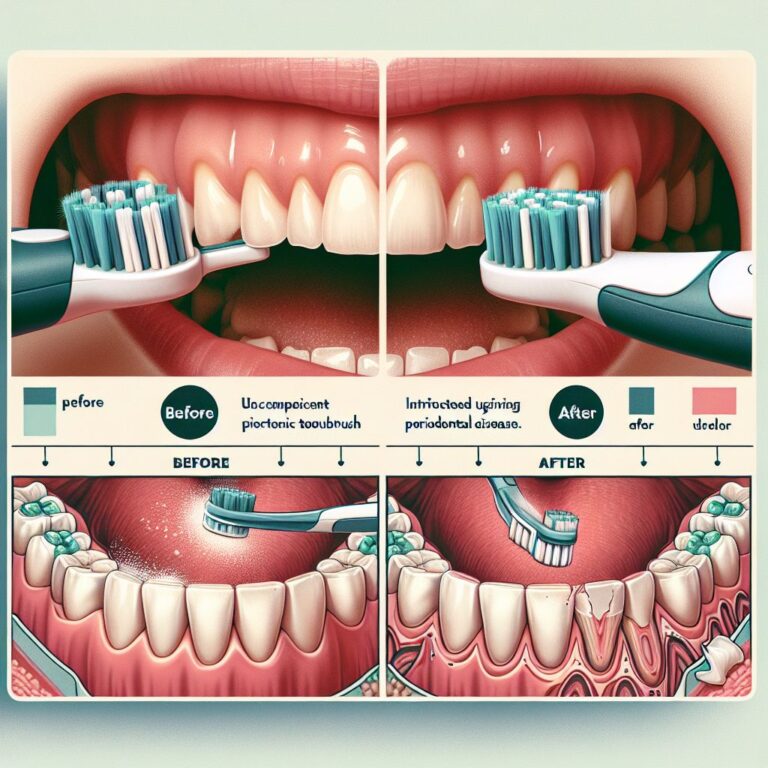
Clinical evidence most strongly supports light therapy’s effectiveness in reducing gingival inflammation and bleeding. Studies consistently show that proper application of photodynamic therapy can significantly decrease bleeding on probing, which indicates active inflammation. Patients with persistent gingivitis despite good mechanical cleaning often see the most noticeable benefits, as the light can reach bacteria in areas brushing and flossing might miss.
Another well-documented benefit is the reduction of harmful bacteria in periodontal pockets. The combination of photosensitizing agents with specific light wavelengths has been shown to reduce bacterial loads by up to 99% in treated areas. This bacterial reduction can help control active infections and potentially slow disease progression in patients with periodontitis.
For individuals with recurring periodontal issues despite good home care and regular professional cleanings, light therapy offers a valuable additional tool. The most compelling success stories typically come from patients with moderate periodontitis who use light therapy consistently as part of a comprehensive treatment approach.
Conditions That Won’t Respond to Light Treatment
Despite enthusiastic marketing claims, several oral conditions show limited or no response to light therapy. Advanced bone loss from long-standing periodontitis cannot be reversed with light therapy alone. Once bone support has been lost, rebuilding typically requires surgical intervention or other regenerative procedures that light therapy cannot replace.
Similarly, structural issues like deep periodontal pockets exceeding 6-7mm typically require professional mechanical cleaning that reaches the pocket base. Light therapy may help maintain results after professional treatment but cannot substitute for the necessary mechanical debridement. Additionally, tooth mobility resulting from advanced periodontal disease won’t stabilize from light therapy alone without addressing the underlying bone loss.
It’s also important to note that cosmetic concerns like tooth discoloration or alignment issues won’t respond to light therapy. Some marketing materials imply broader aesthetic benefits than the technology can deliver, leading to consumer disappointment.
Comparing Results to Traditional Dental Care
The most realistic approach to light therapy is viewing it as a complement to traditional dental care rather than a replacement. Clinical studies consistently show that the best outcomes occur when light therapy is combined with proper mechanical cleaning, both professional and at-home. When compared directly, professional scaling and root planing still outperforms light therapy alone for treating periodontitis.
However, the combination of traditional treatments with adjunctive light therapy frequently yields better results than either approach alone. One systematic review found that patients receiving both scaling and root planing plus photodynamic therapy showed an additional 0.53mm reduction in pocket depth compared to scaling and root planing alone—a modest but clinically significant improvement.
The most balanced perspective recognizes light therapy as one tool in a comprehensive approach to gum health rather than a miracle solution. Regular dental check-ups, professional cleanings, daily brushing and flossing, and addressing risk factors like smoking remain the foundation of periodontal health.
How to Use Light Therapy Devices Properly
The effectiveness of gum health light therapy depends significantly on proper application techniques. Even the most advanced devices will deliver suboptimal results if used incorrectly. Following manufacturer guidelines and understanding the principles behind effective treatment are essential for maximizing benefits.
Most home devices come with detailed instructions, but general best practices can help you get the most from your investment. Consistency and proper technique matter more than occasional intensive use.
Recommended Treatment Frequency
For most gum light therapy devices, daily use shows the best results, particularly during initial treatment phases. Clinical studies typically employ treatment protocols ranging from once daily to three times weekly, with more frequent application generally producing better outcomes for active gum disease. For the Lumoral dual-light system, the manufacturer recommends daily 10-minute treatments, ideally after evening brushing when the mouth will remain undisturbed for several hours. After achieving initial improvements (typically 2-4 weeks), some patients can maintain results with less frequent treatments of 3-4 times weekly, though this varies based on individual risk factors.
Proper Application Techniques
Before using any light therapy device, thorough mechanical cleaning is essential. Brushing and flossing help remove surface plaque that could otherwise block light penetration to deeper tissues. For systems using photosensitizing rinses, follow the specific timing instructions—typically rinsing for 30-60 seconds before light application to allow the compound to adhere to bacterial biofilms.
Position the mouthpiece as directed, ensuring it contacts both upper and lower arches evenly. Most devices have timers that automatically shut off after the recommended treatment duration, typically 8-12 minutes. During treatment, remain relaxed with minimal mouth movement to maintain proper light positioning. Some systems recommend slightly different head positions during treatment to ensure complete coverage of all oral areas.
Complementary Oral Care Practices
Light therapy works best when integrated into a comprehensive oral care routine. Continue regular brushing (at least twice daily) with a soft-bristled toothbrush and fluoride toothpaste. Daily flossing or interdental brushing remains essential, as these mechanical cleaning methods remove plaque in areas where light therapy alone is insufficient. Using an antimicrobial mouth rinse containing ingredients like chlorhexidine or essential oils may provide additional benefits when used at different times of day from light therapy sessions.
Dietary considerations also play a role in maximizing light therapy benefits. Reducing sugary foods and beverages helps limit bacterial fuel sources, while adequate hydration supports overall gum health. For patients with inflammation-driven periodontal issues, an anti-inflammatory diet rich in omega-3 fatty acids and antioxidants may complement the anti-inflammatory effects of certain light wavelengths.
Is Light Therapy Worth Your Money?
Cost-Benefit Analysis: With premium devices like Lumoral costing $500-1,000+ and requiring ongoing purchase of photosensitizing solutions, patients should weigh potential benefits against significant investment. For those with recurrent or resistant periodontal disease despite good conventional care, the cost may be justified by reduced professional treatment needs over time. However, those with mild gingivitis might achieve similar results with improved mechanical cleaning at a fraction of the cost.
The value proposition of light therapy devices varies dramatically depending on your specific oral health situation. For individuals with persistent periodontal issues despite good home care and regular professional treatment, these devices may offer meaningful benefits that justify their substantial cost. Several case studies document patients who reduced the frequency of scaling and root planing procedures after incorporating light therapy into their daily routine.
However, for those with mild gingivitis or healthy gums seeking preventive benefits, the high cost of these devices may exceed their practical value. Improving conventional home care routines and maintaining regular dental visits would likely provide comparable or superior outcomes at lower cost for these individuals.
When evaluating whether to invest in a light therapy device, consider your dental history, risk factors for periodontal disease, and response to conventional treatments. Patients with family history of early tooth loss from periodontal disease, those who smoke, or individuals with diabetes may derive greater benefit from these supplemental approaches.
Ultimately, the decision should involve consultation with your dental professional, who can assess your specific situation and advise whether the potential benefits justify the investment for your particular case. Many dental practices now offer in-office light therapy, which might provide a cost-effective way to test your response before committing to a home device purchase.
Frequently Asked Questions
As light therapy for gum health gains popularity, patients naturally have questions about its applications, limitations, and practical considerations. The following answers address the most common inquiries based on current scientific understanding and clinical experience.
Can light therapy replace regular dental cleanings?
No, light therapy cannot replace professional dental cleanings. While it can reduce bacterial loads and inflammation between visits, it cannot remove calcified deposits (tartar) that form on teeth. These hardened deposits require mechanical removal by dental professionals using specialized instruments. For more information on the benefits and limitations of light therapy, you can read about red light therapy.
Light therapy works best as a complement to regular professional care, potentially extending the benefits of cleanings and helping maintain results between appointments. Some patients with well-controlled periodontal conditions may be able to extend the interval between professional cleanings with consistent light therapy use, but this should only be done under dental professional guidance.
How long does it take to see results from gum light therapy?
Most patients notice initial improvements within 1-2 weeks of consistent daily use, particularly regarding gingival bleeding and inflammation. Visible changes typically begin with reduced bleeding during brushing and flossing, followed by improved gum color as inflammation subsides.
More significant improvements in measurable parameters like probing depths typically require 4-8 weeks of consistent treatment. A case report published in dental journals documented a patient with severe periodontitis who showed significant probing depth reductions after 8 weeks of daily dual-light aPDT treatment combined with mechanical cleaning.
Individual results vary considerably based on several factors, including:
- Severity and duration of existing periodontal disease
- Consistency of light therapy application
- Quality of complementary mechanical cleaning
- Individual immune response and healing capacity
- Presence of risk factors like smoking or diabetes
Are these devices safe for children and pregnant women?
Most manufacturers do not recommend light therapy devices for children under 12 years of age due to limited safety data in pediatric populations and concerns about proper application. For adolescents with gingivitis, supervision by both parents and dental professionals is advisable. Regarding pregnancy, most manufacturers recommend avoiding light therapy during pregnancy and lactation as a precautionary measure, not because of known risks. The photosensitizing agents used in some systems have not been specifically tested for safety during pregnancy, so a conservative approach is warranted until more data becomes available.
Do dental insurance plans cover light therapy devices?
Currently, most dental insurance plans do not cover at-home light therapy devices for gum health. These are typically considered elective or investigational treatments rather than established standard of care. Some dental discount plans may offer reduced pricing on certain devices, but full coverage is rare.
Professional in-office light therapy treatments sometimes receive partial coverage under certain insurance plans, particularly when documented as an adjunct to scaling and root planing for periodontitis treatment. Coverage varies widely between providers and specific plans.
For those with Health Savings Accounts (HSAs) or Flexible Spending Accounts (FSAs), light therapy devices prescribed by a dental professional for specific periodontal conditions may qualify as eligible expenses, though documentation requirements vary by plan administrator.
| Payment Option | Typical Coverage for Light Therapy | Requirements |
|---|---|---|
| Traditional Dental Insurance | Rarely covers home devices; may partially cover in-office treatments | Prior authorization and documented periodontal disease |
| HSA/FSA Accounts | May qualify with professional recommendation | Prescription or letter of medical necessity |
| Dental Discount Plans | Sometimes offers reduced pricing | Varies by specific plan |
If you’re considering purchasing a light therapy device, check with both your dental insurance provider and the device manufacturer about potential reimbursement options or available payment plans.
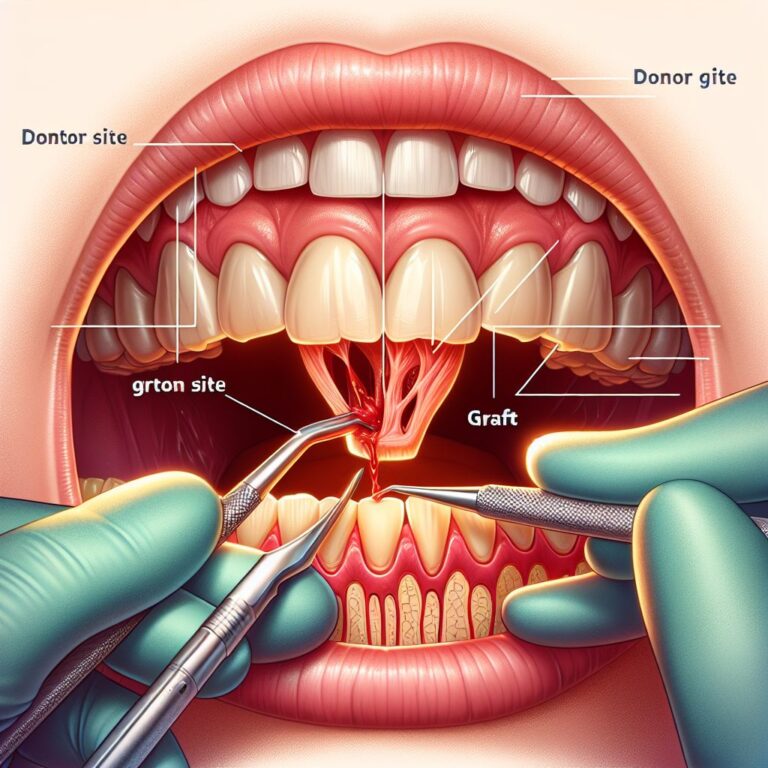
Can light therapy help with gum recession?
Light therapy has limited effect on established gum recession. Once gingival tissue has receded, exposing tooth roots, light therapy alone cannot regenerate lost tissue or restore the original gum line. True gum recession treatment typically requires surgical approaches like gum grafting or guided tissue regeneration performed by periodontists.
However, light therapy may help prevent further recession by addressing underlying inflammation that contributes to ongoing tissue loss. By reducing bacterial load and inflammatory processes in the gingival tissues, certain light therapy protocols may help stabilize existing recession and slow progression, particularly in cases where inflammation is the primary driver rather than mechanical factors like aggressive brushing.
For optimal results with recession concerns, light therapy should be combined with addressing contributing factors such as improper brushing technique, occlusal (bite) issues, or habitial teeth clenching. A comprehensive approach supervised by dental professionals typically yields the best outcomes for managing and preventing further gum recession.