Key Takeaways
- Gum grafting procedures carry specific risks including infection, tissue rejection, bleeding complications, pain issues, and aesthetic concerns that patients should understand before treatment.
- Pre-surgical screening and proper candidate selection significantly reduce complication rates for gum grafting procedures.
- Advanced microsurgical techniques and specialized grafting materials can minimize risks while improving healing outcomes.
- The first 72 hours after surgery are critical for successful graft healing, with specific care instructions that must be followed precisely.
- Colorado Gum Care’s specialized approach to periodontal procedures helps minimize traditional gum grafting risks through enhanced techniques and personalized care protocols.
Gum recession doesn’t just affect your smile’s appearance—it exposes vulnerable tooth roots and can lead to sensitivity, decay, and even tooth loss if left untreated. While gum grafting effectively addresses these issues, understanding the potential risks ensures you’re making an informed decision about your oral health. At Colorado Gum Care, we believe transparency about treatment risks is just as important as highlighting the benefits.
Our periodontal specialists have performed thousands of successful gum grafting procedures, developing advanced techniques that significantly minimize the risks associated with traditional approaches. We’ve found that patients who understand both the benefits and potential complications of their procedure experience less anxiety and better healing outcomes overall.
What Really Happens During Gum Grafting (And Why Risks Matter)
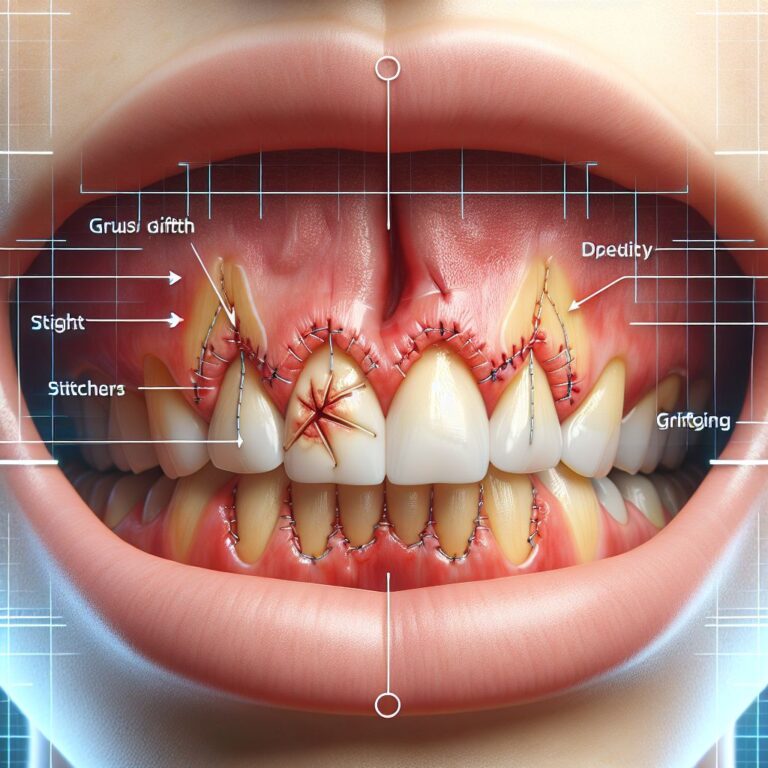
Gum grafting involves transferring soft tissue from one area of your mouth (typically the palate) to cover exposed tooth roots where gum recession has occurred. The procedure itself requires precision microsurgery techniques to ensure proper blood flow to the transplanted tissue and secure attachment to the recipient site. Understanding this delicate process helps explain why certain risks exist and how we work to minimize them.
During a traditional connective tissue graft, the most common type, a small flap is created in the roof of your mouth, and connective tissue is harvested from beneath this flap. This tissue is then carefully positioned over the exposed root surfaces and secured with fine sutures. Alternative approaches include free gingival grafts (taking tissue directly from the palate surface) and pedicle grafts (repositioning nearby gum tissue without creating a separate donor site).
The success of your graft depends on multiple factors: the skill of your surgeon, your oral and overall health, how well you follow post-operative instructions, and the surgical techniques employed. Each of these elements presents potential risk factors that experienced periodontists actively work to control.
5 Major Gum Grafting Risks You Should Know About
While gum grafting is considered safe and predictable in experienced hands, understanding potential complications helps you recognize warning signs and take appropriate preventive measures. The following risks, though uncommon, deserve consideration before undergoing your procedure.
1. Infection: Signs, Prevention, and Treatment
Infection represents one of the primary concerns following any surgical procedure, including gum grafts. Your mouth naturally contains numerous bacteria that could potentially compromise healing at either the donor or recipient site. The classic signs of infection include increased pain after the initial recovery period, unusual swelling that worsens after 48 hours, pus formation, fever, or a foul taste or odor from the surgical site.
To minimize infection risk, we implement a comprehensive approach that includes thorough pre-surgical cleaning, antiseptic mouth rinses, carefully controlled surgical environments, and in some cases, preventive antibiotics. Most importantly, we provide detailed home care instructions that dramatically reduce infection rates when followed correctly.
- Maintain excellent oral hygiene while avoiding the surgical sites
- Use prescribed antimicrobial mouth rinses as directed
- Complete your full course of antibiotics if prescribed
- Avoid smoking and tobacco products completely during healing
- Attend all follow-up appointments for professional monitoring
2. Tissue Rejection and Graft Failure
Unlike organ transplants between different individuals, gum grafts use your own tissue, eliminating true “rejection” risk. However, graft failure can occur if the transplanted tissue doesn’t receive adequate blood supply or becomes damaged during healing. Factors that increase failure risk include smoking (which severely restricts blood flow), poor oral hygiene, certain medical conditions affecting healing, and trauma to the surgical site during recovery. For more information on this topic, visit Colorado Gum Care.
3. Bleeding Complications: Normal vs. Concerning
Some bleeding is expected immediately following gum graft surgery, but should diminish significantly within the first 24 hours. Applying gentle pressure with gauze typically controls minor bleeding. However, persistent or heavy bleeding that doesn’t respond to pressure may indicate a more serious issue requiring immediate attention. Patients taking blood-thinning medications face higher bleeding risks, which is why we carefully review your complete medication history before surgery.
We minimize bleeding complications through precise surgical techniques, appropriate use of hemostatic agents during surgery, and carefully tailored post-operative instructions. For patients with known bleeding disorders or who take anticoagulant medications, we coordinate with your physician to develop a safe surgical plan that may include temporarily adjusting medications under medical supervision.
4. Pain and Sensitivity Issues
Most patients experience mild to moderate discomfort following gum grafting that gradually improves over the first week. However, severe or worsening pain, especially after the third day, may indicate complications like infection or graft failure. The donor site (usually the palate) often causes more discomfort than the grafted area itself. Long-term sensitivity issues can occur if the graft doesn’t properly adhere or if underlying nerve tissue was affected during surgery.
Our pain management protocol includes pre-emptive pain medication, specialized dressings for donor sites, and customized recovery plans. We’ve found that patients who understand what to expect regarding normal discomfort levels experience less anxiety and better pain control. Remember that while discomfort is temporary, the benefits of successful gum grafting last for years.
5. Aesthetic Outcome Problems
While functional success is our primary goal with gum grafting, aesthetic outcomes matter tremendously, especially for grafts in visible areas. Potential aesthetic complications include color mismatches between the grafted tissue and surrounding gums, uneven gum margins, or visible scarring. These issues may result from technique limitations, individual healing characteristics, or inadequate tissue available for grafting.
We address aesthetic concerns through careful pre-surgical planning, digital smile design when appropriate, and selecting graft techniques most likely to provide natural-looking results for your specific situation. In some cases, minor revision procedures can enhance aesthetic outcomes after the initial graft has fully healed.
How Our Advanced Techniques Minimize Your Risk
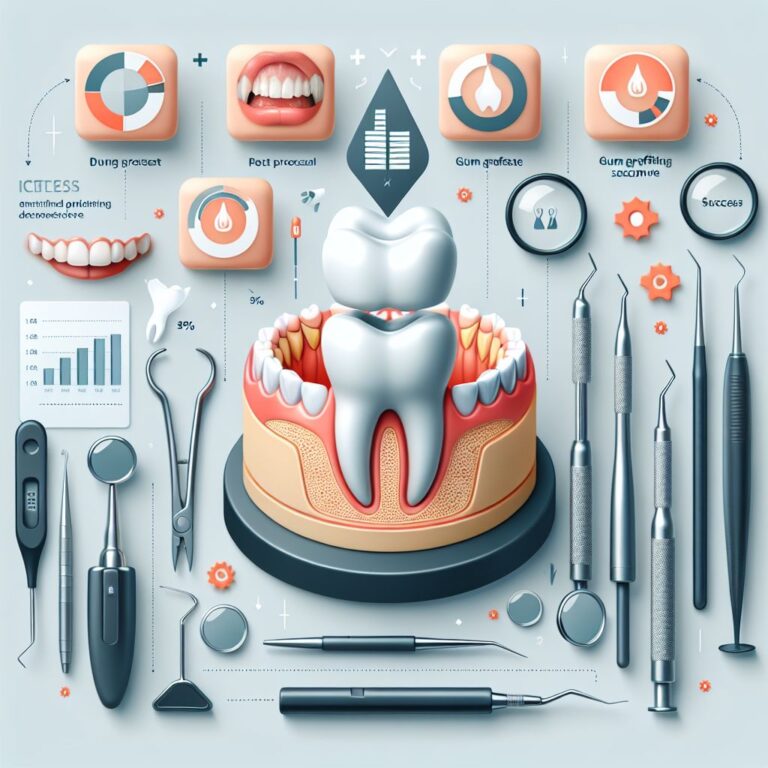
- Comprehensive pre-surgical evaluation and risk assessment
- Microsurgical techniques using magnification and specialized instruments
- Use of platelet-rich fibrin (PRF) to accelerate healing
- Minimally invasive donor site harvesting
- Personalized post-operative care protocols
The foundation of our approach to risk minimization begins with staying at the forefront of periodontal advances. Our practitioners regularly participate in continuing education focused specifically on soft tissue grafting techniques, ensuring our patients benefit from the most current evidence-based approaches. This commitment to excellence translates directly to better outcomes and reduced complication rates.
One significant advancement we’ve implemented is the pinhole surgical technique, which allows us to address gum recession without traditional grafting in suitable cases. This minimally invasive approach eliminates donor site complications entirely while achieving excellent coverage of exposed roots. For cases still requiring traditional grafting, we’ve refined each step of the procedure to minimize trauma and enhance healing.
Our sedation options further contribute to risk reduction by allowing complete relaxation during your procedure. This not only improves your comfort but also enables more precise surgical execution without the complications that can arise from patient movement or anxiety-induced physiological responses.
Pre-Surgical Screening That Makes All The Difference
Before recommending gum grafting, we conduct a thorough assessment that goes beyond just examining your gums. We evaluate your overall health history, medication use, lifestyle factors like smoking, and your healing capacity. This comprehensive screening helps identify risk factors that might compromise your results, allowing us to either address these issues before surgery or modify our approach accordingly. Our digital imaging technology also enables precise planning, ensuring we select the most appropriate grafting technique for your specific situation.
Superior Grafting Materials We Use
- Autogenous tissue (your own tissue) – highest success rates
- Platelet-rich fibrin (PRF) – enhances healing and integration
- Biocompatible membranes – protect grafts during healing
- Growth factors – stimulate tissue regeneration
- Microsurgical sutures – minimize tissue trauma
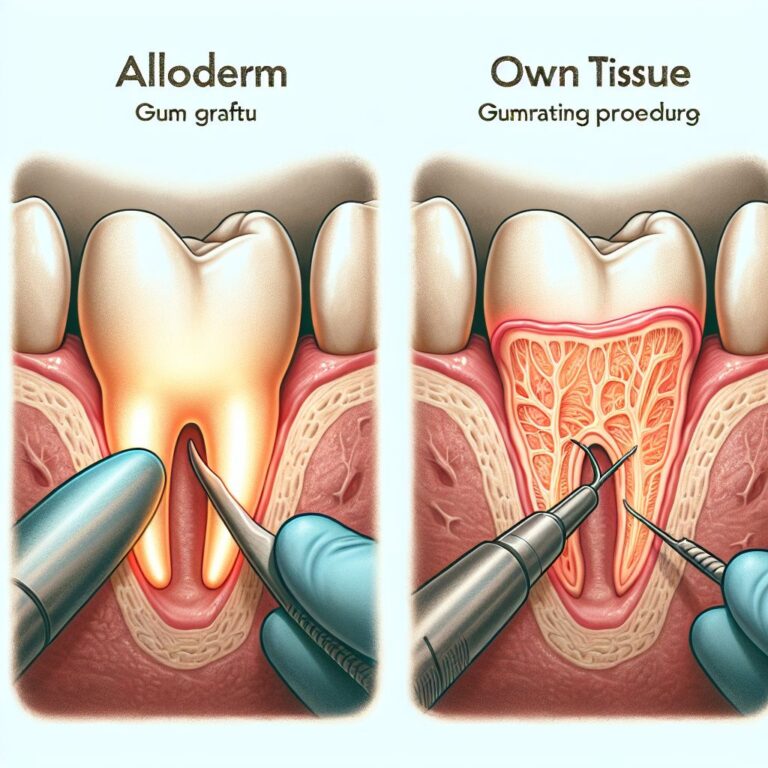
The materials used during your graft significantly impact both your comfort and outcome. We prioritize using your own tissue (autogenous grafts) whenever possible, as these provide the most predictable results with the lowest risk of complications. However, we recognize that minimizing donor site discomfort is equally important, which is why we’ve developed techniques that require smaller tissue samples while maximizing coverage.
For patients with insufficient donor tissue or those who prefer to avoid palatal harvesting, we offer carefully selected alternatives that have demonstrated excellent clinical outcomes. These include allograft materials (processed donor tissue) that undergo rigorous safety protocols to eliminate any disease transmission risk while providing an effective grafting solution.
Our use of platelet-rich fibrin (PRF) represents a significant advancement in graft success rates. This material, created from a small sample of your own blood, concentrates natural growth factors that accelerate healing and enhance tissue integration. PRF application has been shown to improve graft success rates while reducing recovery time and discomfort.
Microsurgical Approach for Better Results
Traditional gum grafting techniques have evolved dramatically with the introduction of microsurgical principles. Using specialized instruments and magnification, we perform grafting procedures with unprecedented precision, resulting in less trauma, faster healing, and more predictable outcomes. This approach allows for finer suturing techniques, more precise tissue manipulation, and better preservation of critical blood supply to both donor and recipient sites. The result is not only reduced risk of complications but also significantly improved aesthetics, with grafts that blend naturally with surrounding tissues.
The Recovery Process: What To Expect and Warning Signs
Successful recovery from gum grafting requires understanding what constitutes normal healing versus potential complications. The healing timeline progresses through distinct phases, each with its own considerations and milestones. Most patients return to normal activities within a few days, though complete healing of the graft takes several weeks. Being familiar with this process helps you distinguish between expected discomfort and signs that warrant contacting our office.
First 72 Hours: Critical Care Instructions
The initial three days following your gum graft procedure are absolutely critical to long-term success. During this period, the transplanted tissue is establishing its blood supply and beginning the integration process with surrounding tissues. Any disruption to this delicate process can compromise your results. That’s why we provide extremely specific care instructions that must be followed meticulously during this time.
- Apply cold compresses as directed to minimize swelling
- Take all prescribed medications exactly as instructed
- Avoid disturbing the surgical sites completely – no brushing, flossing or touching
- Maintain a soft, cool diet avoiding the surgical areas
- Avoid strenuous activities that could increase bleeding
- No smoking or alcohol consumption whatsoever
The protective dressing placed over your graft serves a crucial purpose during these initial days. It shields the delicate tissue while it establishes a blood supply and begins attaching to the recipient site. If this dressing becomes dislodged, contact our office immediately for guidance. Some patients experience minor bleeding during the first 24 hours, which typically responds to gentle pressure with gauze. However, heavy or persistent bleeding requires prompt attention.
Week 1-2: Healing Milestones
As you progress into the first and second weeks of recovery, you’ll notice gradual improvements in comfort and healing. Swelling typically peaks around day three before gradually subsiding. By the end of the first week, most patients experience significant reduction in discomfort and can resume many normal activities with appropriate precautions. During your follow-up appointment (typically scheduled 7-10 days after surgery), we’ll remove any non-dissolving sutures and evaluate your healing progress.
The donor site on the palate often heals more slowly than the graft site itself, forming a yellowish-white tissue layer that’s part of the normal healing process. Complete healing of the palate typically takes 2-3 weeks. During this time, continue following our modified oral hygiene instructions, gradually reintroducing gentle brushing and flossing as directed while avoiding the surgical sites until given clearance.
When To Call Us Immediately
Warning Signs Requiring Immediate Attention:
• Severe, worsening pain not controlled by medication
• Heavy bleeding that doesn’t stop with pressure
• Significant swelling that continues to increase after 72 hours
• Pus or discharge from surgical sites
• Fever over 101°F or chills
• Dressing or significant portions of the graft becoming dislodged
Our commitment to your successful recovery doesn’t end when you leave our office. We provide 24/7 emergency contact information and encourage you to reach out promptly if you experience any concerning symptoms. Early intervention for potential complications dramatically improves outcomes and can often salvage a graft that might otherwise fail. Remember that what seems like a minor issue could signify a developing complication that’s easier to address early.
Patient Success Stories: Before and After
The true measure of any periodontal procedure is found in the experiences of patients who’ve undergone treatment. We’ve had the privilege of helping thousands of patients restore their gum health and confidence through successful grafting procedures. While each case presents unique challenges, our comprehensive approach consistently delivers excellent functional and aesthetic outcomes, even for patients who initially presented with severe recession or complex oral health issues.
- Sarah M. – Received grafting for 6 lower anterior teeth with 90% root coverage after suffering aggressive recession from orthodontic treatment
- Michael T. – Underwent pinhole technique with PRF for maxillary premolars, eliminating sensitivity and improving aesthetics
- Jennifer K. – Treated with connective tissue grafting for a single prominent canine, resulting in complete coverage and elimination of root sensitivity
- Robert P. – Received multiple grafts to address recession caused by aggressive brushing, with excellent tissue matching and no recurrence after 5 years
What these success stories share is not just the technical achievement of coverage, but the positive impact on patients’ quality of life. Many report elimination of sensitivity that had previously made eating and drinking uncomfortable. Others describe newfound confidence in their smile after addressing aesthetic concerns from visible root exposure. Perhaps most importantly, these patients have protected their long-term oral health by preventing further recession and potential tooth loss.
During your consultation, we can share appropriate before and after photos of cases similar to yours, giving you realistic expectations for what can be achieved. While individual results naturally vary based on your unique oral anatomy and the extent of recession, our advanced techniques consistently produce outstanding outcomes even in challenging cases that might be considered difficult to treat elsewhere.
Your Next Steps: Is Gum Grafting Right For You?
Determining whether gum grafting is appropriate for your situation begins with a comprehensive evaluation by our periodontal team. During this consultation, we’ll assess the extent of your recession, identify underlying causes, discuss your health history, and explain all available treatment options. This personalized approach ensures you receive the most appropriate recommendation based on your specific needs rather than a one-size-fits-all solution. We believe informed patients make better decisions, which is why we take time to thoroughly educate you about both the benefits and potential risks of any recommended procedure.
Frequently Asked Questions
Throughout our years of specializing in periodontal care, we’ve found that patients often share similar concerns about gum grafting procedures. Addressing these common questions helps demystify the process and alleviates unnecessary anxiety. Remember that while these general answers provide helpful information, your specific situation may have unique considerations that we’ll discuss during your consultation.
We encourage you to bring your own questions to your appointment, as thorough understanding contributes significantly to successful outcomes. Our team is committed to ensuring you feel completely informed and comfortable with your treatment plan.
How painful is gum graft surgery compared to other dental procedures?
Most patients report that gum grafting discomfort is comparable to having a deep cleaning or filling, though experiences vary based on individual pain tolerance and the extent of your procedure. During the surgery itself, you’ll be comfortably numb and can opt for additional sedation if desired. Post-operative discomfort typically peaks during the first 48 hours and gradually improves over the first week. The donor site on the palate often causes more discomfort than the grafted area itself. Our pain management protocol includes both prescription and over-the-counter medications that effectively control discomfort for the vast majority of patients.
What percentage of gum grafts fail, and why?
In experienced hands using modern techniques, gum grafting has a success rate exceeding 90%. The most common causes of graft failure include smoking (which severely restricts blood flow), poor oral hygiene, traumatizing the graft during healing, and certain underlying health conditions that impair healing. Failure rates are significantly higher among smokers – studies show up to 4-5 times greater risk – which is why we strongly advise completely avoiding tobacco products for at least two weeks before and after your procedure.
At our practice, we track outcomes carefully and maintain failure rates well below national averages through comprehensive pre-surgical screening, advanced surgical techniques, and meticulous follow-up care. When complications do arise, early intervention often allows us to salvage the graft and achieve successful outcomes despite initial challenges. For more information on our procedures, visit our services page.
Can I eat normally after gum graft surgery?
Your diet will require modification during the initial healing period. For the first 1-2 weeks, focus on soft, cool foods that require minimal chewing and won’t disturb the surgical sites. Excellent options include yogurt, cottage cheese, smoothies, mashed potatoes, pasta, eggs, and fish. Avoid anything hard, crunchy, spicy, acidic, or extremely hot in temperature, as these can traumatize healing tissues or cause discomfort.
We provide a comprehensive dietary guide with specific recommendations for each stage of healing. Most patients can gradually return to their normal diet after the second week, though you should continue avoiding extremely hard foods directly contacting the grafted area until given clearance at your follow-up appointment. Proper nutrition actually supports healing, so maintaining adequate calorie and protein intake remains important despite dietary restrictions.
How long until I see the final results of my gum graft?
While you’ll notice improvements in coverage within the first few weeks, the final aesthetic and functional results of gum grafting develop gradually over 3-6 months. Initially, the grafted tissue may appear slightly raised and redder than surrounding gums. As healing progresses, the tissue will flatten and develop color that better matches adjacent tissues. The most significant changes occur during the first month, with more subtle refinements continuing over subsequent months. For more detailed information on gum grafting procedures, you can explore further resources.
Complete integration of the graft, including formation of a functional attachment to the tooth surface, takes approximately 2-3 months. During this time, the tissue gains strength and stability while developing a more natural appearance. We schedule follow-up appointments at key intervals to monitor this process and ensure your healing remains on track. Most patients are delighted to discover that their final results continue to improve even beyond their early post-surgical appearance.
Are there alternatives to traditional gum grafting I should consider?
Several alternatives to traditional connective tissue grafting exist, each with its own benefits and limitations. The pinhole surgical technique allows us to reposition existing gum tissue without harvesting a graft, offering reduced discomfort and faster recovery for suitable candidates. Allograft materials (processed donor tissue) eliminate the need for a palatal donor site while still providing effective root coverage. For minor recession, guided tissue regeneration using specialized membranes and growth factors can sometimes stimulate your body’s natural healing processes without traditional grafting.
Not all alternatives are appropriate for every situation. Factors including the extent and location of your recession, tissue thickness, and underlying causes all influence which approach will provide optimal results. During your consultation, we’ll discuss which options are most suitable for your specific needs, explaining the advantages and potential limitations of each. Our recommendation will balance effectiveness, comfort, long-term stability, and your personal preferences.
At Colorado Gum Care, we specialize in providing the most advanced periodontal treatments available, including minimally invasive options for gum recession. Our team’s expertise in the full spectrum of grafting techniques ensures you receive care tailored precisely to your needs, with the highest probability of success and comfort. Contact us today to schedule your comprehensive evaluation and discover your best path to restored gum health.