Key Takeaways
- Gum grafting tissues come from three main sources: your own mouth (autografts), human donors (allografts), and animal-derived materials (xenografts)
- Palatal tissue from your own mouth remains the gold standard for gum grafts, offering excellent healing and integration
- Acellular dermal matrix (ADM) from human donors eliminates the need for a second surgical site and is carefully processed to remove all cells while maintaining structural integrity
- Animal-derived graft materials undergo rigorous processing to ensure safety and have become increasingly popular alternatives
- Your periodontist will select the most appropriate graft material based on factors including graft size, number of treatment sites, and your specific health considerations
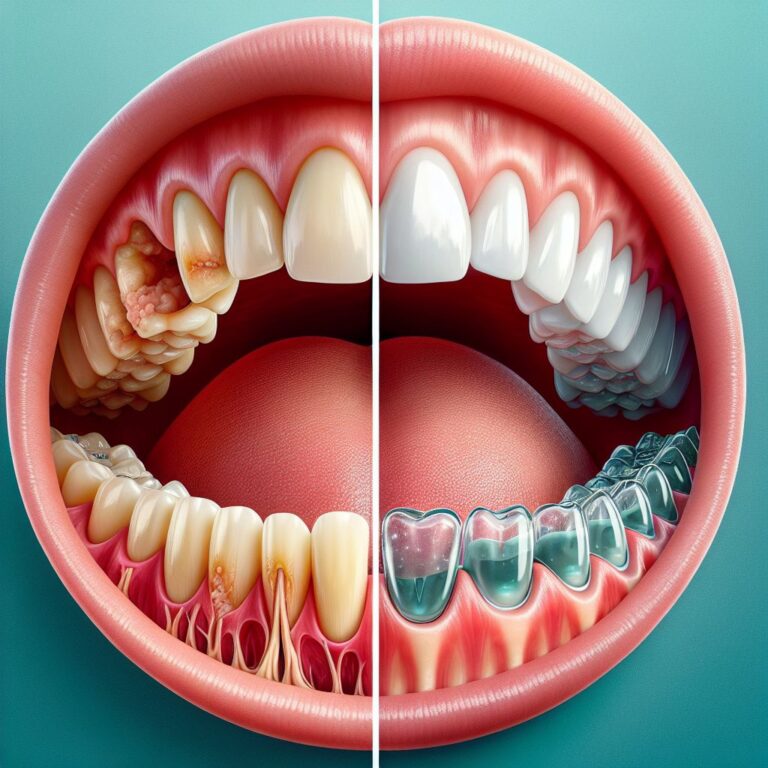
Gum recession can leave tooth roots exposed, leading to sensitivity, increased decay risk, and an aged appearance. Fortunately, modern dentistry offers effective solutions through gum grafting procedures. One of the most common questions patients ask is about where these graft tissues come from – and for good reason.
Understanding your gum grafting options helps you make informed decisions about your oral health. As dental health professionals dedicated to patient education, we believe transparent information about tissue sources leads to better outcomes and reduced anxiety. Let’s explore the different donor tissue options available for gum grafting procedures.
The 3 Main Sources of Gum Graft Tissue You Should Know
When it comes to gum grafting procedures, the tissue used can come from three distinct sources. Each option has specific benefits and considerations that might make it more suitable for your particular situation. Your periodontist will recommend the best option based on your specific clinical needs.
Autografts: Tissue from Your Own Mouth
Autografts involve harvesting tissue from one area of your mouth and transplanting it to the area requiring treatment. Typically, this tissue comes from the roof of your mouth (palate) which has an abundant supply of keratinized tissue similar to healthy gums. This approach is considered the gold standard because it eliminates any risk of tissue rejection or disease transmission. The downside is that it requires two surgical sites – one for harvesting and one for placement – which can increase discomfort during recovery.
Allografts: Human Donor Tissue
Allografts utilize tissue from human donors that has been carefully processed to remove all cells while preserving the collagen structure. These grafts, often called acellular dermal matrix (ADM), are meticulously screened and sterilized according to strict FDA protocols. The major advantage is avoiding a second surgical site in your mouth, resulting in less post-operative discomfort. These materials provide a scaffold for your own cells to populate and eventually transform into your natural gum tissue.
Xenografts: Animal-Derived Tissue
Xenografts are derived from animal sources, most commonly bovine (cow) or porcine (pig) tissue. Like human donor tissue, these materials undergo extensive processing to remove all cellular components, leaving only the collagen matrix. The processing eliminates any risk of disease transmission or rejection. These materials have been used successfully for decades in various medical applications and provide good structure for your own tissue to grow into.
Your Own Tissue: The Gold Standard for Gum Grafts
Using your own tissue for gum grafting offers several distinct advantages that make it the preferred option in many clinical situations. Despite requiring an additional surgical site, the superior healing and tissue integration often make it worth considering.
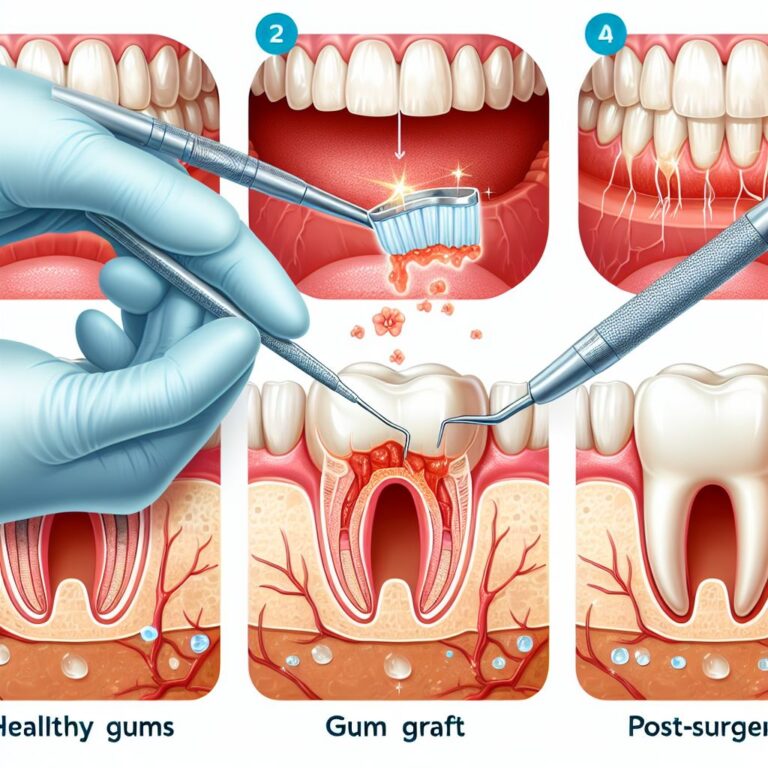
Palatal Tissue: What It Is and How It’s Harvested
The palate (roof of your mouth) contains thick, fibrous tissue that closely resembles healthy gum tissue. During the harvesting procedure, your surgeon removes a small piece of this tissue, carefully selecting the appropriate thickness and size needed for your graft. The palatal donor site is then sutured and typically heals within 1-2 weeks. Modern techniques have significantly reduced discomfort associated with palatal harvesting, though you may experience some soreness similar to a pizza burn during the healing period.
Free Gingival Grafts vs. Connective Tissue Grafts
When using your own tissue, periodontists employ two main techniques. Free gingival grafts involve taking all layers of the palatal tissue, including the visible outer layer (epithelium). This technique creates a patch of thicker tissue that looks somewhat different from surrounding gums initially but provides excellent protection. Connective tissue grafts, on the other hand, use only the deeper layer from beneath the surface, leaving the outer layer intact at the donor site. This method offers better esthetic results as the graft blends more naturally with surrounding tissue.
Benefits: Why Surgeons Often Prefer Your Own Tissue
Using your own palatal tissue provides several distinct advantages. Your body recognizes this tissue as its own, eliminating any risk of rejection or disease transmission. The integration is typically superior, with excellent blood vessel formation (revascularization) occurring more rapidly. Additionally, your own tissue brings living cells to the recipient site, which can accelerate healing and provide better long-term stability. For cases requiring significant tissue thickness or those with challenging recipient sites, autografts often yield the most predictable results.
Another significant benefit is the ability to harvest precisely the tissue characteristics needed for your specific situation. Your periodontist can select the exact thickness, size, and type of tissue required to address your unique needs. For more information on available services, visit Colorado Gum Care.
Limitations: When Your Own Tissue Isn’t Enough
Despite being the gold standard, palatal tissue grafts do have limitations. The most obvious is that your palate has a finite amount of donor tissue available. For patients requiring extensive grafting across multiple sites, there simply may not be enough tissue available. Additionally, the need for a second surgical site increases recovery time and postoperative discomfort. Some patients may have anatomical limitations, such as a thin palate, that make harvesting adequate tissue challenging or impossible.
Medical conditions like bleeding disorders or certain medications may also make palatal harvesting riskier. In these cases, alternative donor sources become necessary options.
Acellular Dermal Matrix: Human Donor Tissue Explained
When using your own tissue isn’t feasible or desirable, acellular dermal matrix (ADM) derived from human donors offers an excellent alternative. This innovative material has revolutionized soft tissue grafting by providing a ready-to-use scaffold for your body’s natural regeneration process.
How Cadaver Tissue Is Processed for Dental Use
Human donor tissue undergoes a sophisticated multi-step process to prepare it for grafting. First, the tissue is carefully harvested from screened donors. It then undergoes a decellularization process that removes all cellular components while preserving the essential collagen structure. This critical step eliminates any potential for disease transmission or immune rejection while maintaining the beneficial scaffold properties of the tissue matrix.
The processing also removes epidermis, dermal cells, and all other cellular components. What remains is a clean, biocompatible collagen framework that your body can incorporate and revitalize with your own cells. The final product is then precisely sized and shaped for dental applications before being sterilized and packaged.
FDA Safety Standards and Sterilization Methods
Human donor tissues adhere to rigorous FDA regulations throughout sourcing, processing, and distribution. All potential donors undergo comprehensive screening for transmissible diseases including HIV, hepatitis, and other pathogens. The tissues themselves are tested using sensitive nucleic acid testing technology to ensure safety. Multiple sterilization methods may be employed, including gamma irradiation, electron beam processing, or proprietary chemical treatments that eliminate potential pathogens while preserving the tissue’s structural integrity.
Why You Only Need One Surgical Site
One of the most significant advantages of using ADM is eliminating the need for a second surgical site. This means no palatal wound to manage during recovery, significantly reducing post-operative discomfort and complications. Many patients report faster recovery times and less pain when ADM is used instead of autografts.
The convenience of having only one surgical site becomes particularly important for patients requiring extensive grafting procedures or those with low pain tolerance. Recovery becomes more straightforward without the need to manage two healing areas simultaneously.
Additionally, eliminating the palatal donor site means no restrictions on the amount of tissue available for grafting. This is especially valuable when treating multiple areas of recession or extensive grafting needs.
- Reduced post-operative pain compared to autografts
- Unlimited supply of graft material for extensive cases
- Faster surgical procedure time
- No need to consider palatal anatomy limitations
- Excellent healing characteristics with predictable results
The simplified recovery process often translates to greater patient satisfaction and willingness to proceed with necessary treatment, particularly for those who might otherwise delay treatment due to fears about pain or recovery time.
When Human Donor Tissue Is the Better Option
Human donor tissue becomes the preferred choice in several clinical scenarios. Patients requiring extensive grafting for multiple teeth can benefit from the unlimited supply of ADM, rather than depleting their own limited palatal tissue. For those with thin palates or anatomical limitations, ADM eliminates concerns about insufficient donor tissue. Patients with medical conditions that increase surgical risks or those taking medications that affect wound healing often benefit from the single-site approach.
Additionally, patients with high dental anxiety or pain sensitivity may find ADM a more acceptable treatment option since it significantly reduces post-operative discomfort. The predictable outcomes and reduced chair time also make it appealing for both clinicians and patients with busy schedules.
Animal-Sourced Graft Materials: A Valid Alternative
Xenografts derived from animal sources have become increasingly popular in periodontal procedures. These materials offer unique advantages while maintaining excellent safety profiles and successful clinical outcomes when used appropriately.
Bovine and Porcine Tissue Processing
Animal-derived graft materials primarily come from porcine (pig) or bovine (cow) sources. The tissue undergoes rigorous processing to remove all cellular components and potential antigens that could trigger immune responses. The resulting acellular collagen matrix provides an excellent scaffold for your body’s cells to populate and regenerate new tissue.
The processing methods vary by manufacturer but typically involve a combination of physical, chemical, and enzymatic treatments to isolate the collagen structure while eliminating all cellular material. The final product retains the beneficial three-dimensional architecture that supports cell migration and tissue regeneration.
Safety Protocols That Protect Patients
Xenografts adhere to strict safety protocols regulated by both the FDA and international standards organizations. Source animals are carefully screened and come from controlled herds maintained specifically for medical applications. The processing methods include validated sterilization techniques that eliminate potential pathogens while preserving the collagen structure needed for successful grafting.
These materials have been used successfully in medicine and dentistry for decades with excellent safety records. The rigorous processing eliminates any risk of disease transmission or allergic reactions, making them suitable options for most patients.
Ideal Scenarios for Using Animal-Derived Grafts
Animal-derived materials excel in certain clinical situations. They’re particularly useful for augmenting thin tissues around dental implants or when creating a zone of attached gingiva. Their predictable thickness and handling properties make them excellent for standardized procedures. For patients with religious or personal objections to human donor tissues, properly processed animal-derived materials may be more acceptable.
These materials also integrate well with various bioactive molecules and growth factors, allowing for enhanced healing in complex cases. Their widespread availability and established track record make them reliable options in the gum grafting armamentarium.
How Your Dentist Decides Which Graft Material to Use
Selecting the optimal graft material involves careful consideration of multiple factors. Your periodontist will evaluate your specific clinical needs alongside personal factors to recommend the most appropriate option for your situation.
Size of the Graft Area
The extent of recession directly influences material selection. Small, localized areas may be ideally treated with autogenous tissue for optimal esthetics and function. Larger areas or multiple sites might benefit from donor materials that eliminate harvest site limitations. Your periodontist will assess the dimensions of recession and the amount of tissue needed to achieve the desired outcome.
The thickness of tissue required also factors into the decision. Some cases require the substantial thickness that only palatal tissue can reliably provide, while others may achieve excellent results with thinner donor materials.
Number of Sites Needing Treatment
Patients requiring treatment at multiple sites face additional considerations. Using your own tissue becomes increasingly challenging as the number of treatment areas increases due to limited donor supply. For extensive cases involving several teeth, ADM or xenografts often become the practical choice, providing consistent quality across all treatment sites without depleting your palatal tissue.
Your Health History and Risk Factors
Medical conditions significantly influence graft selection. Patients with bleeding disorders, compromised immune systems, or those taking medications that affect healing may benefit from approaches that minimize surgical trauma. Donor materials that eliminate the need for palatal harvesting can reduce risks for these patients. Additionally, smoking status, diabetes control, and overall health all factor into the decision-making process.
Previous treatment responses also guide material selection. If you’ve had successful results with a particular graft type in the past, this may influence future recommendations.
Recovery Considerations
Recovery expectations and your ability to manage post-operative care factor into graft selection. Palatal harvesting requires careful attention to the donor site during healing. If you have a low pain threshold or concerns about managing two surgical sites, donor materials may be preferable. Your work schedule, upcoming events, and ability to follow post-operative instructions all influence the ideal approach for your specific situation.
Cost Differences Between Graft Options
Financial considerations inevitably factor into treatment decisions. Autogenous grafts typically involve higher surgical fees due to the additional time and complexity of harvesting tissue. However, they don’t require the purchase of donor materials. Conversely, ADM and xenografts eliminate the harvesting procedure but include material costs. Insurance coverage varies significantly, with some plans covering certain materials but not others. Your dental team can help navigate these financial aspects to find the most appropriate solution for your clinical needs and budget.
What to Ask Your Periodontist About Gum Graft Materials
Open communication with your periodontist is essential for making informed decisions about your treatment. Understanding your options and the reasoning behind recommendations helps ensure you’re comfortable with your care plan.
Before your procedure, schedule a consultation specifically to discuss graft material options. Come prepared with questions about the benefits and limitations of each approach for your specific case. Don’t hesitate to ask about your periodontist’s experience with different materials and their typical outcomes.
Remember that what works best for one patient may not be ideal for another. Your unique clinical situation, personal preferences, and health history all factor into finding the optimal approach for your needs.
Key Questions About Safety and Success Rates
Ask your periodontist about the safety profile of recommended materials. For donor tissues, inquire about screening protocols and processing methods. Understanding success rates for different materials in cases similar to yours provides valuable context for decision-making. Discuss realistic expectations for healing times and long-term outcomes with each option.
It’s also worth asking about the periodontist’s personal experience with different materials. An experienced clinician can often share insights about which approaches have yielded the best results in their practice for cases similar to yours.
Understanding Your Personal Options
Request a thorough explanation of why particular materials are being recommended for your specific case. Discuss how factors like the extent of recession, tissue thickness needs, and your health history influence these recommendations. Don’t hesitate to ask about alternatives if you have concerns about the proposed approach.
Making an Informed Decision Based on Your Specific Case
Take time to consider all the information before making your decision. Ask for before-and-after photos of similar cases with different materials to help visualize potential outcomes. Discuss recovery expectations in detail, including pain management strategies and activity restrictions for each option. For more detailed guidance, explore various services offered to better understand your options.
Remember that your comfort with the treatment plan is important. If you have concerns or questions, your periodontist should be willing to address them thoroughly before proceeding with treatment.
Frequently Asked Questions
Patients often have specific concerns about gum graft materials that extend beyond the general information provided during consultations. Addressing these common questions can help alleviate anxiety and build confidence in the treatment process.
The following questions represent those most frequently asked by patients considering gum grafting procedures. Understanding these aspects of treatment can help you approach your procedure with realistic expectations and confidence.
Important Note: While donor tissues undergo rigorous safety protocols, it’s always important to disclose any allergies or sensitivities to your periodontist before treatment. Though extremely rare, individual reactions can occur. Your provider should monitor your healing process carefully regardless of which graft material is used.
Your periodontist should welcome these and any other questions you may have about your specific situation. Clear communication leads to better outcomes and more comfortable experiences throughout the treatment process.
Is donor tissue for gum grafts as effective as my own tissue?
Current research shows that properly processed donor tissues (both human and animal-derived) achieve comparable clinical outcomes to autografts in many situations. While autografts remain the gold standard for certain applications, donor materials demonstrate excellent success rates in appropriate cases. The key difference lies in healing time rather than final results – your own tissue typically integrates slightly faster due to its living cellular components.
The effectiveness depends largely on proper case selection. Your periodontist will recommend the material most likely to succeed based on your specific clinical needs. For some applications, such as increasing tissue thickness around implants or treating multiple recession sites, donor materials may actually be preferable to autografts.
Long-term studies show that once fully healed, grafted areas function similarly regardless of tissue source. The critical factor is the skill and experience of your periodontist in selecting and placing the appropriate material for your specific situation.
- Autografts may integrate slightly faster due to living cells
- Donor materials achieve comparable long-term results when properly selected
- Some clinical situations actually benefit more from donor materials
- Surgical technique and proper case selection influence outcomes more than material choice
- Both approaches show excellent long-term stability when properly performed
Can disease be transmitted through donor gum graft material?
The risk of disease transmission through properly processed donor materials is virtually non-existent. Human donor tissues undergo extensive screening, testing, and processing that eliminates all cellular components while preserving the beneficial collagen structure. This processing removes any potential for disease transmission. Similarly, animal-derived materials undergo rigorous processing that renders them completely acellular and sterile. All donor materials must meet strict FDA safety standards before being approved for use in patients.
Will my body reject donor tissue used in a gum graft?
True rejection of properly processed graft materials is extremely rare. The processing methods used for both human and animal-derived tissues remove the cellular components that typically trigger immune responses. What remains is primarily a collagen scaffold that your body recognizes as a framework for your own cells to populate. Rather than rejecting the material, your body gradually replaces it with your own tissue through a process called creeping substitution.
- Processing removes cellular components that trigger immune responses
- Remaining collagen scaffold is biocompatible with human tissues
- Your body’s cells gradually replace the scaffold material
- True immunological rejection is exceptionally rare
- Most complications relate to infection or poor healing rather than rejection
It’s important to distinguish between true rejection and other complications like infection or poor healing. Issues with graft integration are more commonly related to local factors such as wound contamination, excessive tension, or inadequate blood supply rather than immunological rejection.
Your periodontist will carefully evaluate your health history for any factors that might affect graft integration and take appropriate precautions to ensure the best possible outcome.
How much of my own tissue can be safely harvested for grafting?
The amount of tissue safely harvestable from your palate depends on several factors including palatal thickness, anatomy, and the specific harvesting technique. Generally, periodontists can safely harvest grafts 1-1.5mm thick with dimensions of approximately 8-15mm in length and 5-7mm in width from each side of the palate. Larger grafts increase the risk of complications like excessive bleeding or prolonged healing.
Your periodontist will carefully evaluate your palatal anatomy using probing measurements or imaging to determine the maximum safe dimensions for tissue harvesting. For patients requiring extensive grafting across multiple sites, this natural limitation often necessitates either multiple surgeries spaced over time or the use of donor materials to supplement your own tissue.
Does insurance cover different types of gum graft materials?
Insurance coverage for gum grafting varies significantly between providers and plans. Most dental insurance plans cover at least a portion of gum grafting procedures when deemed medically necessary to treat gum recession, though coverage percentages and annual maximums vary widely. The specific graft material used may affect coverage, with some plans imposing different benefits for autografts versus donor tissues.
Predetermination of benefits is highly recommended before proceeding with treatment. Your dental office can submit a treatment plan to your insurance provider to obtain an estimate of coverage. Some practices offer financing options or payment plans to help manage out-of-pocket expenses for portions not covered by insurance.
When evaluating costs, consider not just the immediate expense but also the long-term value of proper treatment. Addressing gum recession helps prevent more costly complications like tooth loss or bone damage that could require more extensive treatment in the future.
For comprehensive information about your gum grafting options and personalized recommendations based on your unique situation, schedule a consultation with a periodontist who can evaluate your specific needs. Taking this step toward addressing gum recession can protect your oral health for years to come.
For more information about donor tissue options for gum grafting and to discover which approach might be best for your specific needs, contact our team of dental specialists who can provide personalized guidance based on the latest techniques and materials.