Key Takeaways
- Not all dental implant procedures require tooth extraction, though severely damaged teeth typically need removal before implant placement
- Different implant types have varying extraction requirements – single tooth implants may preserve adjacent healthy teeth while full-arch solutions often involve multiple extractions
- The timeline between extraction and implant placement ranges from immediate placement to waiting 3-6 months depending on bone quality and healing needs
- Bone grafting is often necessary after extraction to create a stable foundation for dental implants
- Getting a second opinion is crucial when multiple tooth extractions are recommended for implant placement
Considering dental implants but worried about losing your natural teeth? Many patients are surprised to learn that not all implant procedures require tooth extraction. While some scenarios necessitate removal, modern dental techniques from leading implant specialists focus on preserving natural teeth whenever possible.
The relationship between tooth extraction and dental implants depends on your specific oral health situation, the type of implant being placed, and your dentist’s treatment philosophy. Understanding when teeth need to be removed—and when they can be saved—empowers you to make informed decisions about your dental care.
The Truth About Dental Implants and Tooth Extraction
Dental implants are titanium posts surgically placed into the jawbone to replace missing tooth roots. They provide a sturdy foundation for artificial teeth that look, feel, and function like natural teeth. Contrary to popular belief, dental implants don’t automatically mean wholesale tooth removal.
The decision to extract teeth prior to implant placement is based on several factors, including the health of existing teeth, bone quality, and the specific implant solution being considered. While some dental professionals may recommend extensive extractions, especially for full-arch restorations, others prioritize tooth preservation whenever possible.
Modern implantology has evolved significantly, allowing for more conservative approaches that can work alongside natural teeth rather than replacing them entirely. This patient-centered philosophy focuses on maintaining oral structures and only removing teeth when absolutely necessary.
When Tooth Removal Is Necessary for Implants
There are legitimate cases where tooth extraction becomes necessary before implant placement. Understanding these scenarios helps clarify when removal is truly in your best interest rather than merely convenient for the procedure.
Severely Damaged or Decayed Teeth
Teeth with extensive decay or damage that extends below the gumline often cannot be saved through conventional restorative methods like fillings, crowns, or even root canals. When a tooth’s structure is compromised beyond repair, extraction followed by implant placement provides the best long-term solution.
Cracked teeth that extend into the root, teeth with significant vertical fractures, or those with recurrent infections despite previous treatments are prime candidates for extraction. In these cases, attempting to preserve the natural tooth might lead to ongoing pain, infection risk, and eventually tooth loss anyway.
Advanced Periodontal Disease Cases
Periodontal (gum) disease is the leading cause of tooth loss in adults. When this condition progresses to advanced stages, it destroys the supporting bone and connective tissues that hold teeth in place. Teeth with severe mobility (looseness) due to bone loss often need extraction before implant placement.
However, it’s important to note that proper periodontal treatment and maintenance can often save teeth affected by earlier stages of gum disease. A comprehensive evaluation by a periodontist can determine which teeth can be saved and which require removal.
Warning Signs That May Indicate Extraction Is Necessary:
• Severe pain that doesn’t respond to medication
• Extreme tooth mobility (looseness)
• Pus or abscess formation around the tooth
• Bone loss visible on X-rays exceeding 50-60%
• Failed previous root canal treatment
• Vertical root fractures, which may require dental implant surgery
Teeth With Failed Root Canals
Root canal therapy can save infected teeth in many cases, but it isn’t always successful. When a tooth with previous root canal treatment develops a persistent infection, extraction may become necessary. These failed cases often result from undetected root fractures, accessory canals that weren’t treated, or reinfection.
Teeth with failed endodontic (root canal) treatment can sometimes be retreated, but when infection persists or the tooth structure is compromised, extraction followed by implant placement offers a more predictable outcome. Your endodontist and restorative dentist should work together to determine if saving the tooth is still possible.
Types of Dental Implants and Their Extraction Requirements
Not all dental implant solutions require the same approach to tooth extraction. Understanding the different types of implants and their specific requirements can help you navigate treatment options more effectively and know what to expect. For more detailed information, you can explore the dental implant surgery process at Mayo Clinic.
Single Tooth Implants
Single tooth implants are designed to replace individual missing teeth without affecting adjacent healthy teeth. This targeted approach requires extraction only when the specific tooth being replaced is damaged beyond repair. The implant post is surgically placed into the jawbone where the natural tooth root once was, and after healing, an abutment and crown are attached.
For patients with one or several damaged teeth scattered throughout the mouth, single tooth implants offer a conservative approach that preserves natural dentition. This method avoids the unnecessary removal of healthy teeth, maintaining the integrity of your natural smile while addressing specific problem areas.
Multiple Tooth Implants and Bridges
When several adjacent teeth are missing or severely compromised, multiple implants can support a dental bridge. This approach may require extraction of remaining teeth in the treatment area if they’re deemed unsalvageable. However, healthy teeth outside the immediate bridge area can typically be preserved.
Implant-supported bridges offer advantages over traditional bridges by eliminating the need to grind down healthy adjacent teeth for support. Instead, strategically placed implants bear the load, protecting remaining natural teeth from excessive forces and potential damage over time.
Full-Arch Implants (All-on-4/All-on-6)
Full-arch restoration techniques like All-on-4 or All-on-6 typically involve the removal of all remaining teeth in an arch. These revolutionary approaches use four to six strategically placed implants to support an entire arch of fixed prosthetic teeth. The procedure is often recommended for patients with extensive tooth decay, advanced periodontal disease, or numerous failing restorations in a single arch.
While this approach does require multiple extractions, it provides a fixed, non-removable solution that looks, feels, and functions like natural teeth. For patients with severely compromised dentition, this comprehensive treatment can restore both function and aesthetics with relatively few implants.
Implant-Supported Dentures
Implant-supported dentures typically require the extraction of remaining teeth in the treatment arch. These specialized dentures snap onto implants placed in the jawbone, offering significantly improved stability and chewing function compared to conventional dentures. For patients with few remaining teeth that are in poor condition, this option eliminates the need to work around problematic teeth.
The number of implants needed varies, with as few as two implants for lower jaw overdentures and four or more for upper jaw stability. This approach provides removable convenience with implant security, making it a popular choice for edentulous or soon-to-be edentulous patients.
Mini Dental Implants
Mini dental implants (MDIs) feature a smaller diameter than traditional implants and can sometimes be placed in areas with less bone volume. While they still require extraction of the tooth being replaced, their smaller size may allow for placement in areas where conventional implants wouldn’t fit without extensive bone grafting. This can be particularly beneficial for patients with narrow spaces between teeth or reduced bone density.
Tooth-Preserving Implant Options
Modern implant dentistry increasingly emphasizes preservation of natural teeth whenever possible. Several innovative approaches allow implants to coexist with your remaining natural dentition, creating hybrid solutions that maximize oral health.
Implants Next to Healthy Natural Teeth
When implants are placed adjacent to healthy natural teeth, special care is taken to maintain adequate spacing and avoid damage to neighboring tooth roots. Advanced 3D imaging and surgical guides ensure precise implant positioning that respects the biological width needed around natural teeth. This approach preserves the natural teeth while filling gaps from missing teeth with implants.
Implants for Already Missing Teeth
The most conservative implant approach involves placing implants only where teeth are already missing. This strategy requires no extractions and focuses on restoring what’s been lost rather than replacing what remains. For patients with generally healthy remaining teeth but gaps from previous extractions, this approach provides targeted restoration.
The benefits extend beyond avoiding unnecessary extractions. By filling spaces promptly after tooth loss, implants help prevent the bone resorption that naturally occurs when teeth are missing. This preservation of jaw structure supports facial aesthetics and helps maintain the health of remaining natural teeth.
Strategically placed implants can also help distribute biting forces more evenly across your dental arch, reducing stress on remaining natural teeth. This biomechanical advantage helps protect natural teeth from excessive wear and potential fracture.
| Implant Type | Extraction Requirements | Preservation Potential |
|---|---|---|
| Single Tooth Implant | Only the affected tooth | High – preserves adjacent teeth |
| Implant-Supported Bridge | Affected teeth in bridge area | Medium – preserves teeth outside bridge area |
| Full-Arch (All-on-4/6) | Typically all teeth in arch | Low – focuses on full replacement |
| Implant-Supported Dentures | Most/all teeth in arch | Low – designed for edentulous patients |
| Mini Dental Implants | Only affected teeth | Medium-High – can fit in narrower spaces |
Your dentist should thoroughly explain which teeth (if any) need extraction for your specific implant plan and why. This transparency allows you to make fully informed decisions about your oral health and explore alternative options if extensive extractions seem excessive.
Strategic Implant Placement
Advanced implant techniques allow for strategic placement that maximizes support while minimizing the number of implants needed. Techniques like tilted implant placement (used in All-on-4) can avoid anatomical structures like sinuses or nerves while providing sufficient support for full-arch restorations. This approach often reduces the need for bone grafting procedures and can sometimes allow for immediate loading of provisional restorations.
The Controversy of Preventive Extractions
A concerning trend in implant dentistry involves recommending multiple extractions based on potential future problems rather than current conditions. Some practitioners advocate removing teeth that show early signs of disease or minor damage, suggesting that extraction and implant placement now will prevent problems later. While this approach may seem proactive, it raises significant ethical questions about unnecessarily removing salvageable teeth.
Preventive extraction philosophy often frames the decision as inevitable – suggesting patients will eventually lose problematic teeth, so addressing them all at once is more efficient. However, with proper care and maintenance, many teeth with early-stage issues can last decades longer, preserving natural function and bone structure.
When Dentists Recommend Removing Healthy Teeth
Some implant centers propose removing relatively healthy teeth to create space for a full-arch implant solution. This “clean slate” approach may be motivated by technical simplicity, predictability of outcomes, or financial considerations. While full-arch restorations offer excellent solutions for severely compromised dentition, they represent significant overtreatment for patients with mostly healthy teeth.
Red flags include recommendations to extract teeth without symptoms that show only minor radiographic changes, or suggestions that any tooth with a root canal or crown will inevitably fail. Modern dentistry has extensive evidence showing that properly treated and maintained teeth with restorations can function successfully for many years, even decades.
Second Opinion: When to Get One
If your treatment plan includes extracting multiple teeth that aren’t causing pain or infection, seeking a second opinion is strongly recommended. This is especially important if you’re told that all teeth in an arch need removal for implants. A prosthodontist, periodontist, or endodontist can provide specialized evaluation of tooth restorability and help determine which teeth genuinely need extraction versus which can be preserved.
Different dental professionals may have different treatment philosophies. Some focus primarily on implant placement, while others emphasize tooth preservation whenever possible. Getting perspectives from multiple specialists provides a more balanced view of your treatment options and ensures you’re not undergoing unnecessary extractions.
Questions to Ask Your Dentist About Proposed Extractions
- Why specifically does this tooth need to be removed? What evidence supports this recommendation?
- Is this extraction absolutely necessary for implant placement, or are there alternatives?
- What would happen if we tried to save this tooth instead? What would that treatment involve?
- What is the long-term prognosis for this tooth if we attempt to save it?
- Are there any specialists you recommend I consult before proceeding with extraction?
- How will removing this tooth affect my remaining natural teeth and overall oral health?
The Healing Process After Extraction for Implants
Understanding the healing process after tooth extraction provides important context for implant treatment planning. The extraction site undergoes significant changes as it heals, affecting both the timing and approach to implant placement.
Immediate vs. Delayed Implant Placement
Immediate implant placement involves inserting the implant post into the socket immediately after tooth extraction. This approach can reduce overall treatment time and may help preserve bone and gum architecture. However, it requires excellent initial stability of the implant and is not suitable for all cases, particularly those with active infection or insufficient bone.
Delayed implant placement allows the extraction site to heal partially or completely before implant surgery. Early delayed placement typically occurs 2-3 months after extraction, while conventional delayed placement happens 4-6 months after extraction. This approach allows for resolution of infection and initial bone healing, potentially increasing implant success rates in challenging cases.
The decision between immediate and delayed placement depends on factors including bone quality, extraction site condition, aesthetic considerations, and the patient’s overall health. Your dental surgeon will recommend the most appropriate timing based on your specific circumstances.
Bone Grafting Requirements
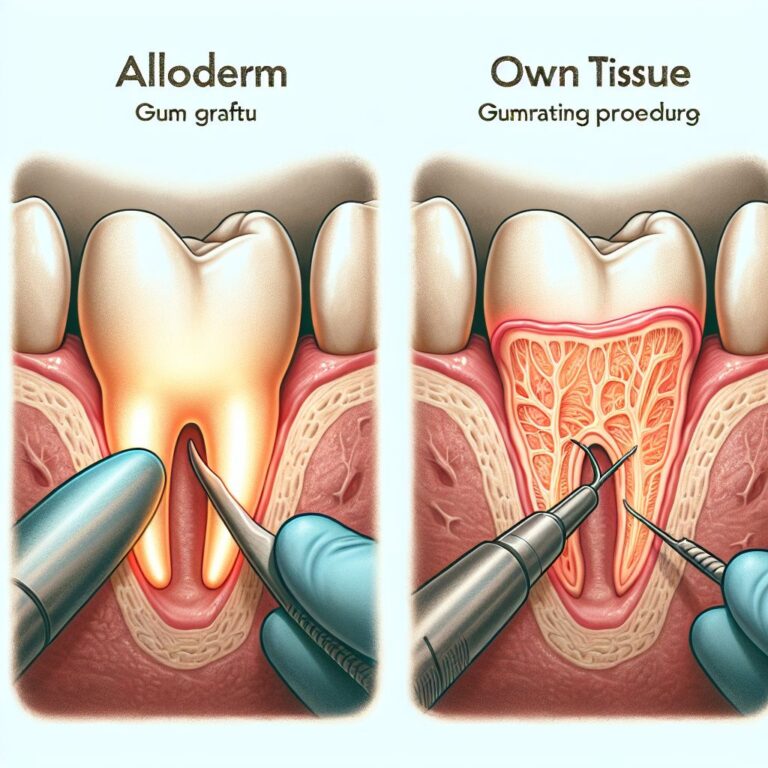
When a tooth is extracted, the surrounding bone naturally begins to resorb or shrink. This process, called ridge resorption, can reduce the available bone volume for implant placement. To counteract this, bone grafting procedures are often performed either at the time of extraction (socket preservation) or before implant placement (ridge augmentation).
Socket preservation involves placing bone graft material directly into the extraction socket to maintain ridge dimensions during healing. This preventive approach reduces the need for more extensive grafting later. Ridge augmentation addresses bone loss that has already occurred, rebuilding the jawbone to create adequate width and height for implant placement.
The type of grafting material used can range from your own bone (autograft) to processed bone from human donors (allograft), animals (xenograft), or synthetic materials. Each has specific advantages and healing characteristics that your surgeon will consider when planning your treatment.
Typical Timeline From Extraction to Final Implant
The complete process from tooth extraction to final implant restoration typically spans several months, though exact timelines vary based on individual healing, treatment approach, and whether bone grafting is needed. For standard cases with delayed placement, patients can expect approximately 3-6 months between extraction and implant placement, followed by another 3-4 months for osseointegration (the process by which the implant fuses with the jawbone).
Immediate placement protocols can reduce the overall timeline, sometimes allowing for provisional restorations on the same day as extraction. However, even with immediate placement, the final restoration usually isn’t attached until the implant has fully integrated with the bone, typically 3-6 months later. For more information on the procedure, visit Mayo Clinic’s dental implant surgery guide.
Patients requiring extensive bone grafting may face longer timelines, with some complex cases taking up to a year from extraction to final restoration. While this extended treatment period can test patience, rushing the process risks implant failure and disappointing results.
Make the Right Choice for Your Dental Health
The decision to extract teeth for dental implants should never be taken lightly. While implants offer an excellent solution for replacing missing teeth, preserving natural teeth whenever possible remains a fundamental principle of good dentistry. Work with dental professionals who thoroughly explain all options, respect your questions, and prioritize conservation of natural structures when feasible. Remember that your oral health is a lifelong journey, and decisions made today will impact your dental future for decades to come.
Frequently Asked Questions
Many patients have similar questions about tooth extraction and dental implants. These answers provide general guidance, though your specific situation may vary.
Can a dental implant be placed without removing my tooth?
No, a dental implant directly replaces a missing tooth root and requires that space in the jawbone. However, if you’re asking whether adjacent or other teeth need to be removed for implant placement, the answer is often no. Single or multiple implants can frequently be placed while preserving surrounding healthy teeth. Only the specific tooth being replaced needs extraction.
Is it better to save my natural tooth or get an implant?
When a natural tooth can be predictably saved through procedures like root canal therapy, periodontal treatment, or restorative dentistry, preservation is typically preferred. Natural teeth maintain proprioception (position sense) and periodontal ligaments that help distribute forces. Even teeth with root canals that are properly restored can function successfully for many years.
However, when a tooth has a poor long-term prognosis due to extensive damage, recurrent infections, or severe bone loss, extraction and implant placement often provides more predictable outcomes. The decision should be based on thorough evaluation of the specific tooth, not blanket recommendations.
How long after tooth extraction can I get an implant?
Implant placement timing varies based on individual circumstances. Immediate placement can occur the same day as extraction in select cases with adequate bone and no active infection. Early placement typically happens 2-3 months after extraction, while conventional delayed placement occurs 4-6 months post-extraction. Cases requiring significant bone grafting may need 6-9 months before implant placement. Your implant surgeon will recommend the appropriate timeline based on your specific situation.
Why might a dentist recommend removing all my teeth for implants?
Complete arch extraction may be recommended in cases of advanced periodontal disease affecting multiple teeth, extensive decay throughout the mouth, or numerous failing restorations with poor prognosis. Full-arch implant solutions like All-on-4 can provide predictable, fixed rehabilitation in these scenarios. However, this approach should only be recommended when most teeth are genuinely unsalvageable, not as a convenient alternative to treating salvageable teeth.
If you’re advised to have all teeth in an arch removed but many appear stable and functional, seeking a second opinion from a prosthodontist or periodontist is strongly recommended. Preserving even a few strategic natural teeth can sometimes improve outcomes and maintain better proprioception.
Does tooth removal for implants hurt more than regular extractions?
Extractions performed in preparation for implants typically don’t cause more discomfort than standard extractions. In fact, they may be performed with extra care to preserve bone and surrounding tissues, which can actually reduce trauma. Most patients report manageable discomfort controlled with prescribed pain medication for a few days after extraction. The surgical technique, your dentist’s expertise, and your individual pain tolerance all influence your experience more than the reason for extraction.
Many implant providers offer sedation options ranging from nitrous oxide to oral conscious sedation or IV sedation for patients concerned about discomfort or dental anxiety. These approaches can make the extraction process more comfortable and reduce stress during treatment.