Key Takeaways
- Gum graft retainers provide crucial protection for both the surgical and donor sites during the recovery period, significantly reducing the risk of complications.
- These clear plastic shields can reduce post-operative pain by up to 60% compared to recovery without a retainer, according to periodontal studies.
- Most patients will need to wear their retainer for 1-2 weeks after surgery, though individual healing timelines vary based on the type of graft performed.
- Proper retainer care, including gentle cleaning and correct positioning, can dramatically improve healing outcomes and overall comfort.
- While initially feeling strange in your mouth, most patients report becoming completely accustomed to their retainer within 48-72 hours.
Recovering from a gum graft can feel like navigating unfamiliar territory. That strange sensation in your mouth, the worry about disturbing the surgical site, and the nagging question of whether you’re doing everything right to ensure proper healing. If your periodontist has mentioned a “retainer” as part of your recovery plan, you might be wondering what exactly that means for your comfort and healing process.
Why Your Gums Need Protection After a Graft
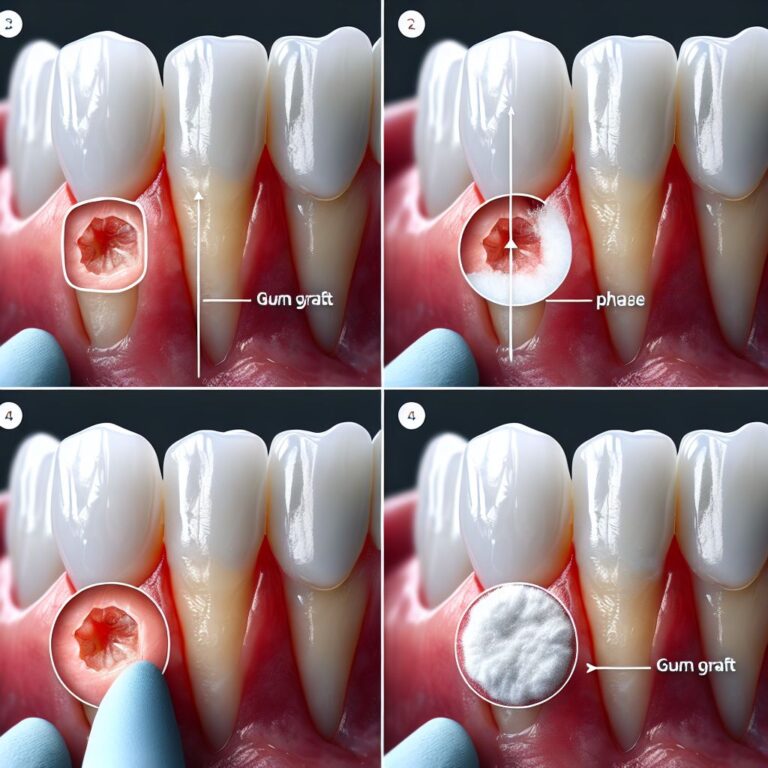
Gum recession exposes the sensitive roots of your teeth, making them vulnerable to decay, sensitivity, and further damage. A gum graft addresses this by taking tissue from one area of your mouth (typically the roof) and attaching it to the area where your gums have receded. This delicate surgical procedure creates two healing sites in your mouth: the recipient site where the new tissue is placed and the donor site where tissue was harvested.
Both these areas are extremely vulnerable during the first days and weeks after surgery. The newly placed graft tissue needs time to establish blood supply and integrate with surrounding tissues. Meanwhile, the donor site (often likened to a pizza burn on the roof of your mouth) is essentially an open wound that requires protection from your tongue, food, and other potential irritants.
Without proper protection, these healing sites face numerous threats. Your tongue may unconsciously probe the areas, food particles can become trapped against the healing tissue, and normal brushing could disrupt the delicate sutures holding everything in place. This is where a gum graft retainer becomes an essential ally in your recovery journey.
What Exactly Is a Gum Graft Retainer?
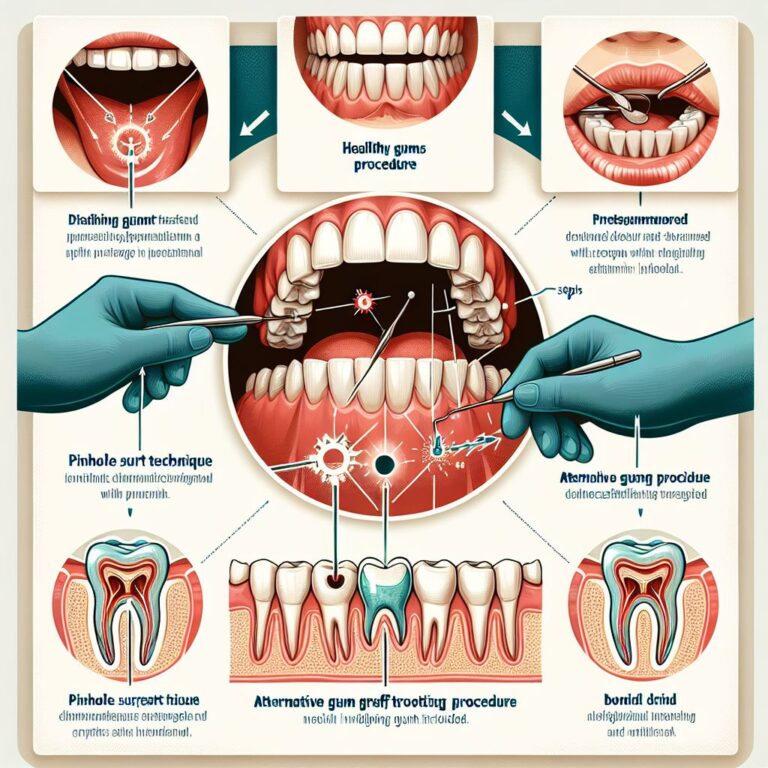
A gum graft retainer is a custom-made, clear plastic shield designed to fit precisely over either the surgical site, the donor site, or both, depending on your specific procedure. Think of it as a protective bubble for your healing gum tissues. Unlike the retainers used after orthodontic treatment that focus on maintaining tooth position, these specialized retainers serve a completely different purpose: they act as barriers between vulnerable healing tissues and the potentially damaging elements in your mouth.
The Clear Plastic Shield That Speeds Recovery
The retainer is typically made from clear, medical-grade plastic or acrylic material that’s been precisely molded to fit your mouth. Your periodontist takes impressions either before your surgery or immediately after, ensuring the retainer will fit comfortably without putting pressure on the surgical sites. The transparency allows your dental professional to monitor healing without removing the device, while the smooth surface prevents food debris from becoming trapped against healing tissues.
Most retainers cover either the palate (roof of the mouth) to protect the donor site or fit over the recipient area where the graft was placed. Some comprehensive designs may protect both areas simultaneously. The edges are carefully smoothed to prevent irritation to your tongue or cheeks, making them surprisingly comfortable once you’ve adjusted to wearing them.
How It Differs From Surgical Putty
Some patients confuse gum graft retainers with surgical putty or dressing, but they serve different functions. Surgical putty is typically a temporary covering placed immediately after surgery that hardens to protect the wound for the first few days. This putty often resembles a pink or white material that feels somewhat like clay or wax in your mouth. For more information on gum graft procedures, you can visit Healthline’s detailed guide.
A retainer, by contrast, is a removable device designed for longer-term protection. While surgical putty may be placed and removed only by your dental professional, you’ll generally be responsible for inserting, removing, and cleaning your retainer during recovery. The retainer offers more substantial protection than putty alone and can be reinserted as needed throughout your healing process.
Additionally, while surgical putty typically falls off or dissolves within days, your retainer remains intact throughout your healing period, providing consistent protection for weeks if necessary. This extended protection is particularly valuable for complex grafts or for patients who’ve had multiple grafting sites treated in a single procedure.
When Your Dentist Will Recommend One
Not every gum graft procedure will require a retainer. Your periodontist’s recommendation will depend on several factors unique to your situation. Patients receiving free gingival grafts or connective tissue grafts (which involve tissue harvested from the palate) are most likely to benefit from palatal retainers to protect the donor site. The size of your graft, the location in your mouth, and your individual risk factors will all influence whether a retainer is recommended.
Patients with professions that involve excessive talking, those who play wind instruments, or individuals who have a history of disturbing healing sites with their tongue may particularly benefit from this additional protection. Similarly, if you’re prone to dry mouth, have a restricted diet that limits soft foods, or simply feel anxious about protecting the surgical site, a retainer can provide both physical protection and peace of mind during recovery.
Your dentist may also recommend a retainer if you’ve experienced complications with previous dental surgeries or if your particular graft presents additional challenges. The goal is always to maximize your comfort while ensuring optimal conditions for successful healing.
5 Major Benefits of Wearing Your Retainer
The decision to use a gum graft retainer isn’t merely about following your periodontist’s instructions—it’s about actively participating in your own healing process. Understanding the specific benefits can help motivate consistent use during those critical first days and weeks after your procedure.
1. Protects the Donor Site From Damage
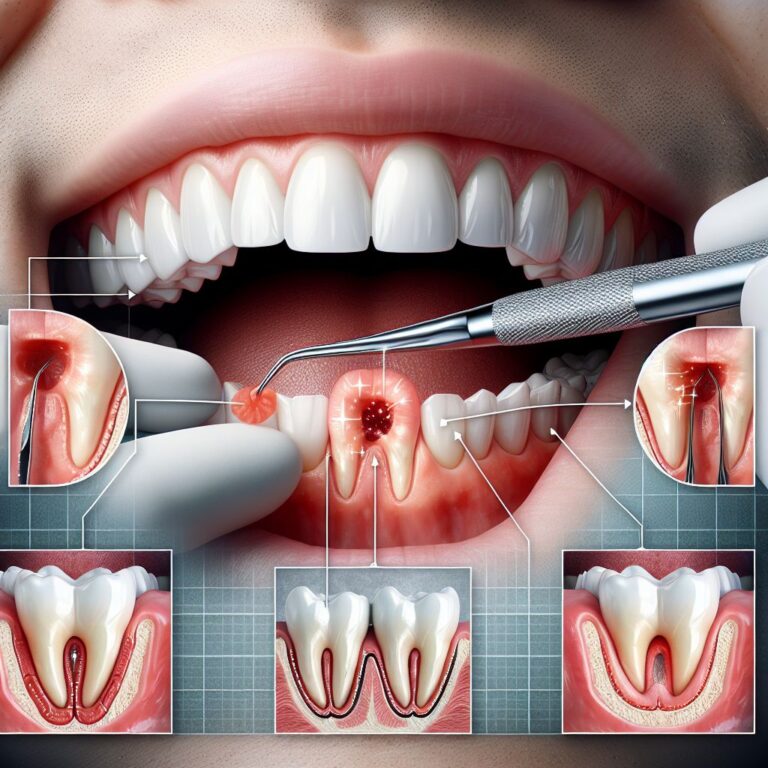
The roof of your mouth, where tissue is typically harvested for connective tissue and free gingival grafts, is extremely sensitive during healing. Each time your tongue moves across this area, it can disrupt the delicate formation of new tissue. Even more concerning, food particles can become trapped against the healing site, increasing the risk of infection and delaying recovery.
A properly fitted retainer creates a physical barrier that prevents both unconscious tongue movements and food debris from interfering with the healing donor site. This protection is particularly valuable during sleep, when you have no conscious control over tongue movements. Studies have shown that protected donor sites typically form a stable protective layer within 7-10 days, compared to 14+ days for unprotected sites.
For patients who’ve undergone procedures harvesting larger amounts of tissue, this protection can significantly reduce the chance of developing painful tissue irregularities or scarring that might cause long-term discomfort. The smooth surface of the retainer also prevents your tongue from constantly “checking” the wound, which many patients do unconsciously.
2. Reduces Pain and Discomfort
Post-operative pain following a gum graft primarily comes from exposed nerve endings at both the donor and recipient sites. Every time these sensitive areas are disturbed—by your tongue, food, or even air passing over them—pain signals fire. A retainer serves as a protective shield that dramatically reduces these painful stimuli.
Many patients report that inserting their retainer provides almost immediate pain relief, especially from the sharp, stinging sensations that can occur when air passes over the donor site. This pain-reducing benefit is particularly noticeable during eating and drinking, when temperature changes and food textures would otherwise cause significant discomfort.
Beyond physical protection, the psychological comfort of knowing your surgical sites are shielded can reduce stress and anxiety during recovery. This mental ease often translates to better sleep, improved appetite, and an overall more positive healing experience. Some periodontists even note that patients who consistently wear their retainers typically request fewer pain medications during recovery.
3. Prevents Infection
Open wounds in your mouth—whether at the donor or recipient site—are naturally vulnerable to the hundreds of bacterial species that normally inhabit your oral cavity. While not all these bacteria are harmful, some can potentially interfere with healing or cause infection if they colonize the surgical sites. A retainer creates a physical barrier that significantly reduces bacterial access to these vulnerable areas.
Additionally, most retainers are designed to allow your periodontist to prescribe antimicrobial rinses that can be applied inside the retainer itself, creating a protected environment with reduced bacterial load. This controlled environment helps maintain optimal conditions for healing while minimizing infection risk. For patients with compromised immune systems or those with diabetes, this infection prevention benefit is particularly valuable.
The retainer also prevents food particles—which can harbor bacteria—from becoming trapped against healing tissues. Without these food particles providing nutrients for bacterial growth, the risk of developing painful infections like dry socket (at extraction sites) or necrosis of the graft tissue is substantially reduced.
4. Makes Eating and Speaking Easier
One of the most immediate challenges after gum graft surgery is returning to normal eating and speaking patterns without disturbing the surgical sites. The retainer creates a smooth protective surface that allows food to glide past sensitive areas rather than directly contacting them. Many patients find they can return to a wider variety of foods more quickly when using a retainer consistently.
For speaking, the retainer helps prevent the painful experience of your tongue repeatedly hitting the donor site on the roof of your mouth when forming certain sounds. While you may notice some minor speech changes while wearing the retainer, most patients find this far preferable to the sharp pain that can occur when the tongue repeatedly contacts an unprotected palatal wound. This benefit is especially important for professionals who speak frequently during their workday.
Some specialized retainers even include design elements that help maintain normal speaking patterns by providing stable reference points for your tongue. Your periodontist can discuss whether these specialized options might be beneficial based on your profession and daily speaking requirements.
5. Speeds Up Healing Time
Perhaps the most compelling benefit of consistent retainer use is the potential for faster overall healing. By maintaining stable conditions around the surgical sites, your body can focus energy on tissue regeneration rather than repeatedly responding to new irritations or minor injuries. Patients who use their retainers as directed typically experience more predictable healing timelines with fewer setbacks.
The protective environment created by the retainer supports the critical early phases of healing when new blood vessels are forming within the graft tissue. This vascularization process, essential for graft survival, progresses more efficiently when the tissue remains undisturbed. Some clinical studies suggest that proper protection can improve graft success rates by 15-20%, particularly for more complex procedures.
Additionally, faster healing means a quicker return to normal brushing and flossing in the affected areas, which further supports long-term gum health. While most patients focus on the immediate recovery, this improved long-term outcome may be the most significant benefit of all.
The Sensation: What to Expect When Wearing Your Retainer
The unfamiliar feeling of a retainer in your mouth after gum graft surgery can initially seem more uncomfortable than the surgery itself. However, understanding what sensations are normal can help ease this transition period. Most patients find that the initial strangeness quickly gives way to relief as they recognize how much the retainer protects sensitive areas.
Your perception of the retainer will evolve significantly throughout your recovery period. What feels bulky and intrusive on day one typically becomes barely noticeable by the end of the first week. This adaptation happens not just because you mentally adjust to the sensation, but because swelling naturally decreases and your mouth physically accommodates to the retainer’s presence.
First 24 Hours: Initial Adjustment Period
During the first day with your retainer, you’ll likely be acutely aware of its presence in your mouth. The smooth plastic surface may feel unusually slick against your tongue, and you might notice increased saliva production as your mouth responds to this foreign object. You may also experience a slight gag reflex when first inserting the retainer, particularly if it extends toward the back of your palate. These sensations are entirely normal and typically subside within hours as your body adapts.
Days 2-3: Getting Comfortable
By the second and third days, most patients report significantly less awareness of the retainer. Your tongue will have begun mapping the new contours of your mouth with the retainer in place, making speech and swallowing feel more natural. The initial saliva overproduction typically normalizes during this period, and any minor soreness from the edges of the retainer usually resolves as your tissues adapt.
During this phase, you’ll likely begin appreciating the protection the retainer provides, especially when eating or drinking. Many patients report feeling anxious when removing the retainer for cleaning because they’ve quickly grown accustomed to the barrier it provides between their tongue and the sensitive surgical areas. This growing appreciation often helps motivate consistent use through the remainder of the healing period.
After One Week: Barely Noticeable
By the end of the first week, most patients report that the retainer feels like a natural extension of their mouth. The initial hyperawareness fades as your brain categorizes the sensation as “background information” rather than something requiring conscious attention. Speech patterns typically return to near-normal during this period as your tongue learns to navigate efficiently around the retainer.
As the donor site begins healing during this period, you may notice that the retainer feels slightly looser or different. This change results from reduced swelling and the formation of new tissue at the surgical sites. Some periodontists may adjust your retainer at your one-week follow-up appointment to ensure it continues providing optimal protection as your mouth changes during healing.
Normal Feelings vs. Warning Signs
While some discomfort is normal when wearing a gum graft retainer, it’s important to distinguish between expected sensations and potential problems. Normal sensations include a feeling of pressure, slight soreness at the edges of the retainer, and awareness of the smooth plastic surface against your tongue and palate. You might also notice some mild tissue blanching (whitening) where the retainer contacts your gums, which typically resolves within minutes after removal.
Warning signs that should prompt a call to your periodontist include sharp pain (rather than pressure or soreness), significant difficulty breathing or swallowing, persistent gagging even after several days of wear, or visible tissue damage where the retainer contacts your mouth. Additionally, if you notice increasing rather than decreasing pain as days pass, or if your retainer suddenly feels dramatically tighter, these could indicate complications requiring professional evaluation.
Daily Life With Your Gum Graft Retainer
Adapting your daily routines to accommodate your gum graft retainer doesn’t have to be complicated. With a few practical adjustments, you can maintain comfort while ensuring optimal protection for your healing tissues. Most patients find that creating simple routines around eating, speaking, and sleeping helps them use their retainer consistently throughout the recovery period. For more information on gum graft recovery, you can refer to this comprehensive guide.
Remember that while the retainer may seem inconvenient initially, the protection it provides significantly reduces your overall recovery time. This makes the temporary adaptations well worth the effort, especially during the critical first week after gum graft surgery when healing tissues are most vulnerable to disruption.
Eating Tips: What Works Best
Your periodontist will provide specific guidance about whether to remove your retainer during meals or keep it in place. This recommendation depends on the location of your graft, the type of procedure performed, and your individual healing progress. If instructed to remove your retainer while eating, do so carefully and place it in its storage case to prevent contamination or damage.
Cold, soft foods are typically most comfortable during the first 48-72 hours after surgery. Options like yogurt, smoothies, ice cream, and chilled applesauce provide nutrition without requiring significant chewing or creating heat that might increase swelling. As healing progresses, you can gradually introduce room-temperature soft foods like mashed potatoes, pasta, and scrambled eggs. For more information on post-surgery care, you can visit Healthline’s guide on gum grafts.
When wearing your retainer during meals (as some periodontists recommend), choose foods that can be easily consumed with minimal chewing. Take smaller bites than usual and chew on the side opposite your graft site whenever possible. Avoid extremely hot foods and drinks, as heat can distort your retainer and potentially increase swelling at the surgical sites.
Talking Without Lisping
Speech adjustments represent one of the most noticeable challenges when wearing a gum graft retainer, particularly for palatal retainers that cover the roof of your mouth. Initially, you may notice a lisp or difficulty pronouncing certain sounds, especially those that require your tongue to contact the roof of your mouth (“t,” “d,” “n,” and “l” sounds).
Practice makes significant difference in adapting your speech. Spending just 5-10 minutes reading aloud each day can dramatically accelerate your adaptation to speaking with the retainer. Focus particularly on problematic sounds, deliberately slowing your speech initially and gradually increasing to normal speed as your tongue learns new movement patterns. For more information on dental care, you can visit Healthline’s guide on gum grafts.
If you have important work presentations or social events during your recovery period, consider practicing key phrases in advance. Most patients find their speech improves dramatically within 2-3 days of consistent retainer wear, with nearly normal speech returning by the end of the first week.
Sleeping Comfortably
Nighttime protection is particularly important for healing gum graft sites, as unconscious tongue movements during sleep can disturb delicate tissues without your awareness. Most periodontists strongly recommend wearing your retainer during sleep throughout your recovery period. Position your head slightly elevated with an extra pillow during the first few nights to reduce swelling and minimize pressure on the surgical sites.
If you normally sleep on your stomach or side, temporarily adjusting to back sleeping may improve comfort while wearing your retainer. This position reduces pressure on your face and minimizes the chance of the retainer shifting during sleep. If you find yourself removing the retainer unconsciously during sleep (which some patients report), consider setting an alarm for mid-night to check and reinsert it if necessary.
Rinsing with cool water before inserting your retainer at bedtime can help reduce any discomfort and create a clean environment for overnight healing. Some patients find that taking any prescribed pain medication approximately 30 minutes before bedtime helps them fall asleep comfortably with the retainer in place.
Proper Care of Your Retainer
Maintaining a clean retainer is essential not only for your comfort but for preventing potential infections during the vulnerable healing period. A well-maintained retainer provides maximum protection while minimizing complications. Establishing a simple cleaning routine helps ensure consistent care throughout your recovery period.
Cleaning Do’s and Don’ts
DO clean your retainer each time you remove it, using cool or lukewarm water to rinse away any debris or saliva. A soft toothbrush designated specifically for your retainer can be used to gently clean the surfaces, particularly the side that contacts your surgical sites. Your periodontist may recommend a specific non-abrasive cleaning solution; common options include mild antimicrobial mouthwash diluted with water or specialty retainer cleaning tablets.
DON’T use hot water on your retainer, as heat can warp the plastic and alter the precise fit that provides optimal protection. Similarly, avoid harsh cleaning chemicals like bleach, alcohol-based mouthwashes at full strength, or abrasive toothpastes, all of which can damage the retainer material or leave residues that might irritate healing tissues. Never boil your retainer or place it in the dishwasher, microwave, or direct sunlight, as these environments can permanently distort the material.
When to Remove It
Your periodontist will provide specific guidance about when to remove your retainer based on your particular procedure and healing progress. Generally, you’ll remove the retainer for gentle cleaning 2-4 times daily during the first week. Some periodontists recommend keeping the retainer in place continuously for the first 24-48 hours, removing it only for prescribed rinses, while others suggest more frequent removal for cleaning from the beginning. For more detailed information, you can visit this gum graft guide on Healthline.
Most protocols involve removing the retainer for cleaning after meals and before bed. However, if you’ve been instructed to wear your retainer while eating, you’ll typically remove it immediately after eating to rinse both your mouth and the retainer before reinserting it. As healing progresses, your periodontist may adjust these recommendations, often allowing more time without the retainer as tissues stabilize.
- First 24-48 hours: Minimal removal, only as specifically directed
- Days 3-7: Remove 3-4 times daily for cleaning and prescribed rinses
- Second week: Gradually increasing time without the retainer, especially during meals
- Beyond two weeks: Often transitioning to nighttime-only wear or complete discontinuation
Always follow your specific post-operative instructions, as these timelines may vary significantly based on your procedure type, healing progress, and individual risk factors. Some patients, particularly those with larger grafts or multiple surgical sites, may need to wear their retainer for extended periods.
How to Insert and Remove Without Pain
Proper technique when handling your retainer can significantly reduce discomfort and prevent accidental damage to healing tissues. To insert your retainer, rinse it thoroughly with cool water, then position it gently over the appropriate area (palate or recipient site). Use light, even pressure with your fingers to seat the retainer fully, rather than pushing with your tongue. If your retainer uses clasps around teeth for retention, position these carefully to avoid pressing on sensitive gum tissues.
For removal, start by relaxing your jaw slightly. Use your fingertips (not fingernails) to gently loosen one edge of the retainer, usually starting from the back or side rather than directly over any surgical site. Once loosened at one point, the retainer should release with minimal pressure. Avoid creating suction by “pulling” the retainer, as this negative pressure could potentially disturb healing tissues. Instead, use a gentle rocking motion to break the seal before removing the retainer completely.
Your Road to Recovery: Timeline and Milestones
Understanding the typical healing progression after a gum graft helps you recognize signs of successful recovery and identifies when you should expect to transition away from retainer use. While individual healing varies based on the type of graft, extent of the procedure, and your personal health factors, most patients follow a relatively predictable recovery pattern with their retainer playing a crucial supportive role throughout the process.
The initial 72 hours represent the most critical period for graft protection, when new blood vessels begin forming between the graft and recipient site. Your retainer provides essential stability during this period. By days 4-7, early tissue integration begins, though the connections remain delicate. The second week typically brings significant strengthening of these connections, often allowing modified retainer wear. By 2-3 weeks post-surgery, most patients have sufficiently stable healing to discontinue regular retainer use, though some may continue wearing it at night for additional protection.
Frequently Asked Questions
Recovery from gum graft surgery brings numerous questions as you navigate this unfamiliar experience. The following answers address the most common concerns patients have about their gum graft retainers. Remember that while these general guidelines apply to most situations, your periodontist’s specific instructions should always take precedence.
If you encounter situations not covered here or experience symptoms that seem unusual, don’t hesitate to contact your dental professional. Most practices welcome these questions and prefer addressing concerns early rather than managing complications later.
How long will I need to wear my gum graft retainer?
Most patients need to wear their gum graft retainer consistently for 1-2 weeks following surgery, with the first week typically requiring nearly continuous wear (except during cleaning). As healing progresses, your periodontist may transition you to wearing the retainer only during sleep or high-risk activities. The total duration depends on your specific procedure, healing progress, and risk factors. Free gingival grafts typically require longer retainer use (often 2+ weeks) than connective tissue grafts, while pedicle grafts sometimes need less protection. Your periodontist will evaluate your healing at follow-up appointments and provide guidance on when you can safely discontinue retainer use.
Can I eat with my retainer in place?
Whether you should eat with your retainer in place depends on your specific procedure and your periodontist’s recommendations. For palatal retainers protecting a donor site, many professionals suggest keeping the retainer in place while eating soft foods to maintain continuous protection. For retainers covering recipient sites, removal during meals is more common to prevent food particles from becoming trapped between the retainer and healing graft.
- Soft, cool foods like yogurt, smoothies, and ice cream are typically easiest to manage with a retainer in place
- Avoid sticky foods that might adhere to or dislodge the retainer
- Take smaller bites and chew slowly, preferably away from surgical sites
- Rinse both your mouth and retainer thoroughly after eating, even if you removed the retainer during the meal
If you’ve been instructed to remove your retainer while eating, clean it immediately before reinsertion to prevent introducing food particles to the surgical sites. Place the retainer in its storage case during meals rather than wrapping it in a napkin, which can lead to accidental disposal or contamination.
As healing progresses, usually after 7-10 days, your periodontist may modify these restrictions to allow more normal eating patterns. This transition typically coincides with the formation of a stable protective layer over the donor site and initial integration of the graft tissue at the recipient site.
Some patients find that certain foods remain challenging throughout the recovery period, particularly those requiring significant chewing or those with small particles that might get trapped under the retainer. Adapting your diet temporarily is a worthwhile trade-off for optimal healing outcomes.
Will the retainer affect my speech?
Yes, you will likely notice some speech changes when first wearing your gum graft retainer, particularly if it covers the palate (roof of your mouth). The tongue uses the palate as a reference point for many speech sounds, so the altered surface temporarily affects your ability to form certain sounds clearly. Most patients experience a noticeable lisp, especially when pronouncing sibilant sounds (s, z, sh) and sounds that require tongue-to-palate contact (t, d, n, l). These speech changes are temporary and improve significantly with practice.
Most patients adapt their speech patterns within 2-3 days of consistent retainer wear, with near-normal speech returning by the end of the first week. If you have professional speaking engagements during your recovery period, consider scheduling them after this initial adaptation phase. Alternatively, practicing specific troublesome words or phrases in advance can help you navigate important conversations more comfortably during the adjustment period.
How do I clean my retainer?
Clean your retainer each time you remove it using cool or lukewarm water and, if recommended by your periodontist, a gentle non-abrasive cleaner. Start by thoroughly rinsing the retainer under running water to remove any visible debris or saliva. You can use a soft toothbrush designated specifically for your retainer to gently clean all surfaces, paying particular attention to any areas that contact surgical sites. Avoid using your regular toothpaste, as many formulations contain abrasives or strong flavoring agents that can damage the retainer material or leave residues that might irritate healing tissues.
Many periodontists recommend soaking the retainer briefly in antimicrobial solution during your recovery period. Options might include diluted alcohol-free mouthwash, specialized retainer cleaning tablets, or prescription antimicrobial solutions. Always rinse the retainer thoroughly with cool water after any soaking treatment and before reinsertion. Store your retainer in its protective case whenever it’s not in your mouth to prevent contamination or damage.
What should I do if my retainer feels too tight or painful?
Some initial pressure sensation is normal when wearing a new gum graft retainer, but significant pain or a feeling that the retainer is “too tight” warrants attention. First, ensure you’re inserting the retainer correctly—improper positioning can create pressure points that cause discomfort. If you’ve verified correct placement and still experience pain, remove the retainer and inspect both it and your mouth for any obvious issues like sharp edges on the retainer or visible irritation in your tissues.
Minor discomfort that doesn’t improve within 24-48 hours of consistent wear should be reported to your periodontist. They may need to adjust the retainer to eliminate pressure points or address changes in your mouth as healing progresses. Never attempt to modify the retainer yourself, as this could alter the protective function and potentially create new problems.
If your previously comfortable retainer suddenly begins feeling tighter or causing pain, this could indicate increased swelling at the surgical sites, which might suggest infection or other complications. In these cases, contact your periodontist promptly for evaluation. They can determine whether the issue requires treatment and make any necessary adjustments to your retainer.
With proper fit and care, your gum graft retainer should enhance your recovery experience rather than detract from it. The temporary adaptations required during healing are well worth the improved outcomes and reduced complications that proper retainer use provides. For personalized guidance about protecting your healing gum tissues, consult with your dental health professional who can provide recommendations specific to your unique situation.